A PAIN IN THE NECK: CROSS-SECTIONAL SURVEY OF WORK-RELATED MUSCULOSKELETAL INJURIES (WR-MSI) IN CYTOTECHNOLOGISTS IN ALBERTA
Rebecca J Brassington (Department of Laboratory Medicine and Pathology, University of Alberta, Edmonton, AB, Canada), Brinda Balachandra (Department of Laboratory Medicine and Pathology, University of Alberta, Edmonton, AB, Canada and Royal Alexandra Hospital, Edmonton, AB, Canada)
Background: Prolonged microscope use is commonly associated with work-related musculoskeletal injuries (WR-MSI), resulting in numerous negative effects. This study examines WR-MSI among Cytotechnologists and other microscope users in Alberta.
Methods: This ethically-approved cross-sectional study investigates the prevalence and impact of WR-MSI in microscope users, along with factors associated with MSI. Survey data were analyzed using SPSS Statistics.
Results: A key finding is that over 85% of all Cytotechnologists reported experiencing WR-MSI. 66% reported injury to their neck, more than any other body site surveyed. Cytotechnologists showed greater effect of WR-MSI than trainees or Pathologists (p< 0.001). This included negative impact on both workplace performance, with decreased productivity and missed work, as well as personal life, with mental health and participation in life outside of work.
Conclusions: This study indicates a high prevalence of WR-MSI and its deleterious effects on work and personal life in microscope-using medical laboratory staff; particularly Cytotechnologists.
Keywords: Microscopy, Ergonomics, Survey, Cytopathology, Cytotechnology
A RARE CASE OF LINGUAL CRYPTOCOCCOSIS PRESENTED AS A TONGUE NODULE IN A HIV-POSITIVE PATIENT
Huynh Thuy Tien Dinh (Pham Ngoc Thach University of Medicine, Ho Chi Minh City, Vietnam), Van Thi Ai Hoang (Hue University of Medicine and Pharmacy, Hue, Vietnam.), Frank Chen (Department of Pathology, University at Buffalo, Buffalo, NY, U.S.A.)
Introduction: Cryptococcus is an opportunistic fungal infection that primarily affects those with advanced HIV/AIDS. Oral manifestations are rare, and involvement of the tongue is exceptionally uncommon. Here, we present a rare case of lingual cryptococcosis.
Clinical Presentation: A 30-year-old male undergoing treatment for cryptococcal meningitis presented with a papillary-like mass on the tongue. Given his history of advanced HIV and former smoking, oral malignancy or infection was initially considered. A subsequent biopsy of the tongue nodule collected firm tan soft tissue fragments.
Results: Histologic evaluation of the mass on H&E staining revealed squamous epithelium with subepithelial tissue containing round to oval yeasts with thick mucoid capsules, amidst mild inflammation. Focal ulceration and bacterial colonies were present on the epithelial surface. No evidence of malignancy can be identified. Periodic Acid-Schiff (PAS) and Grocott Methenamine Silver (GMS) stains highlighted abundant fungal organisms. Mucicarmine decorated the highly characteristic gelatinous capsules with bright pink color, consistent with cryptococcosis.
Conclusion: This rare case of disseminated cryptococcosis involving the tongue in an HIV-positive patient highlights the need to consider fungal infections in atypical oral lesions. Oral cryptococcosis is uncommon and can easily be mistaken for more common conditions, such as neoplasms or bacterial infections. Our findings underscore the importance of considering fungal infections in the differential diagnosis of atypical oral lesions in immunocompromised patients, and reinforce the role of biopsy in guiding timely diagnosis and management.
Keywords: Cryptococcus, Cryptococcosis, HIV, tongue, mucicarmine
A TOUGH NUT TO CRACK: A CASE OF NUT CARCINOMA ARISING IN THE SALIVARY GLAND
Joel Scott (University of Saskatchewan, Department of Pathology and Laboratory Medicine), Javera Tariq (University of Saskatchewan, Department of Pathology and Laboratory Medicine), Nicholas Baniak (University of Saskatchewan, Department of Pathology and Laboratory Medicine), Rani Kanthan (University of Saskatchewan, Department of Pathology and Laboratory Medicine), Steve Angel (University of Saskatchewan, Department of Pathology and Laboratory Medicine), Ryan Campbell (University of Saskatchewan, Department of Pathology and Laboratory Medicine)
Introduction: NUT carcinoma is a rare, aggressive carcinoma defined by NUT gene rearrangements, typically arising in the thorax or sinonasal tract. We present a case of NUT carcinoma arising in the submandibular gland, a rarely reported location for this entity. CLINICAL
Presentation: A 48-year-old female presented with a rapidly enlarging neck mass. An initial ultrasound was performed revealing a left submandibular gland lesion measuring 3.2 x 2.8 x 2.7 cm. Subsequent FNA was negative for malignancy. Clinical progression led to a CT scan demonstrating the left submandibular gland lesion increased to 7.3 x 4.7 x 4.5 cm with evidence of invasion into the neck and regional nodal involvement. Needle core biopsy was arranged, with a primary differential of lymphoma vs salivary gland neoplasm.
Results: The biopsy showed sheets of monotonous, undifferentiated cells with an extensive neutrophilic infiltrate and without foci of squamatization. A broad immunohistochemistry panel was performed showing positive staining for NUT and p63. NUT IHC positivity is highly specific, and in combination with p63, supports the diagnosis of NUT carcinoma. The patient underwent extensive left radical neck dissection for staging, with final pathology results pending.
Conclusion: This case of salivary gland NUT carcinoma is a rare and difficult diagnosis, made possible with a thorough differential and access to modern IHC stains. To our knowledge, 25 cases of NUT carcinoma arising in major salivary glands have been reported in the literature, with this being the 6th arising in the submandibular gland. We hope the continued study of these cases can lead to improved diagnostic and therapeutic options for patients.
Keywords: Head and Neck, NUT carcinoma
ADULT GRANULOSA CELL TUMOUR WITH HIGH-GRADE TRANSFORMATION: A CASE REPORT AND REVIEW OF LITERATURE
Jiaxin Lin (Department of Pathology, University of Manitoba), Sarah Kean (Department of Obstetrics, Gynecology and Reproductive Sciences, University of Manitoba; CancerCare Manitoba Research Institute, CancerCare Manitoba), Esther Ranvinsky (Department of Pathology, University of Manitoba)
Objectives: Adult granulosa cell tumours (AGCT) with high-grade transformation are rare, with only nine cases reported in the current literature. The terminology of “high-grade transformation” is often confused in the context of sarcomatoid transformation in AGCT, which is also rare and poorly documented in the literature. The expression patterns of p53 and TP53 mutations have been linked to high-grade morphological changes in a series of five cases. However, further evidence is needed to clarify this association.
Design/Methods: We investigated p53 expression and TP53 mutation in a case of high-grade AGCT and conducted a literature review.
Results: We present a case of a 44-year-old woman with progressive abdominal distention and pain caused by a large pelvic mass. Histologic examination revealed typical AGCT morphology alongside components of high-grade transformation. Molecular analysis confirmed the AGCT diagnosis by identifying the FOXL2 C134W mutation. TP53 mutations were also detected, exhibiting a null mutation immunohistochemistry (IHC) staining pattern. In conjunction with our case, TP53 mutations were identified in 7 out of 9 primary and recurrent tumours, and p53 IHC mutation patterns were observed in 6 out of 7 primary tumours, indicating a strong association between high-grade transformation in AGCT and TP53 mutations. Lastly, a summary of the literature on AGCT with high-grade transformation and AGCT with sarcomatoid transformation is provided to facilitate better understanding of these entities.
Conclusion: This study highlights a strong association between TP53 mutations and high-grade transformation in AGCT, while also emphasizing the importance of distinguishing high-grade transformation from sarcomatoid transformation.
Keywords: Adult Granulosa Cell Tumour, high grade transformation, TP53 mutation
ALK-REARRANGED SPITZ NEVUS OF THE HARD PALATE: A RARE INTRAORAL PRESENTATION WITH DISTINCTIVE MORPHOLOGIC FEATURES
Huangrui R. Zhu (University of Saskatchewan College of Medicine, Saskatoon, SK, Canada), Amanda Gruza (Saskatchewan Health Authority, Department of Pathology and Laboratory Medicine, Saskatoon, SK, Canada), Katelynn Campbell (Saskatchewan Health Authority, Department of Pathology and Laboratory Medicine, Saskatoon, SK, Canada)
Spitz nevi are uncommon melanocytic proliferations that typically arise in children and adolescents. A subset of these neoplasms harbors ALK gene rearrangements, which correlate with distinctive histopathologic and immunohistochemical features. While ALK-rearranged Spitz nevi are generally benign, they can exhibit features that mimic atypical or malignant melanocytic lesions, particularly when arising in unusual anatomic locations. We report a diagnostically challenging case of an ALK-rearranged Spitz nevus arising on the hard palate, an extremely rare site for this entity. An 11-year-old female with no significant medical history was incidentally found to have a 7-millimeter exophytic red papule on the hard palate during routine orthodontic care. Observation was initially pursued in hopes of spontaneous regression. However, as the lesion persisted, an excisional biopsy was performed. Histopathologic evaluation revealed a well-circumscribed, compound melanocytic proliferation with enlarged spindled to epithelioid melanocytes arranged in vertically oriented fascicles, along with a prominently admixed angiomatoid component. Mitotic figures were visible at up to 2 per square millimeter in the superficial aspect of the lesion. Immunohistochemistry showed diffuse ALK positivity, negative BRAF expression, retained BAP1, and a gradient pattern of HMB-45 staining, confirming an ALK-rearranged Spitz nevus. This case underscores the importance of recognizing the characteristic morphologic and immunophenotypic features of ALK-rearranged Spitz tumours, particularly when arising in uncommon mucosal sites where their presentation may mimic melanoma or other atypical lesions.
Keywords: Spitz, ALK, Melanocytic, Pediatric, Dermatopathology
CERVICAL AND VAGINAL HPV-INDEPENDENT INVASIVE SQUAMOUS CELL CARCINOMAS AND THEIR PRECURSOR LESIONS
Chunyi Tan (Department of Pathology and Molecular Medicine, McMaster University, Hamilton, ON), Naiya Amin (Faculty of Science, McMaster University, Hamilton, ON), Monalisa Sur (Department of Pathology and Molecular Medicine, McMaster University, Hamilton, ON; Department of Oncology, Juravinski Hospital & Cancer Center, McMaster University, Hamilton, ON), Alice Lytwyn (Department of Pathology and Molecular Medicine, McMaster University, Hamilton, ON), Nikfar Nikzad (Department of Pathology and Molecular Medicine, McMaster University, Hamilton, ON)
Objective: HPV-independent squamous cell carcinoma (SCC) of the cervix was included in the WHO Classification of Tumours in 2020. While HPV-independent SCC is well recognized in the vulva, non-vulvar HPV-independent SCCs are rare, and little is known about their precursor lesions. The majority of HPV-independent SCCs are associated with p53 mutations. This study aims to describe the clinicopathologic, immunohistochemical, and molecular characteristics of HPV-independent cervical and vaginal carcinomas and their precursor lesions.
Methods: We prospectively identified HPV-independent SCC cases of the cervix and vagina from 2019 to 2024 at our institution. Cases were evaluated histologically and with p16 immunohistochemistry (IHC) and HPV in situ hybridization (HPV-ISH). p53 IHC was performed to assess for abnormal expression patterns. Clinical follow-up was obtained where available.
Data and Results: Between 2019 and 2024, we identified three cases of HPV-independent cervical SCC and one case of vaginal SCC. Patient ages ranged from 55 to 88 years. The carcinomas measured from 6.3 to 10.4 cm. The histology of the precursor lesions included aberrant maturation with basal atypia (dCIN), as well as features seen in VAM (abundant keratinization and aberrant maturation lacking basal atypia). The carcinomas and precursors were p16 and HPV-ISH negative, and p53 was overexpressed in one case and wild type in the remainder. One patient died 9 months post-surgery with lung metastases, and another at 4 months with progressive lymphadenopathy while on chemotherapy. One patient with lung metastases has started chemotherapy and immunotherapy, and the fourth patient with parametrial invasion is undergoing radiation treatment.
Conclusion: HPV-independent SCC occurs in the cervix and vagina and is associated with HPV-independent precursor lesions histologically similar to those in the vulva. These carcinomas may be associated with abnormal p53 expression.
Keywords: HPV-independent carcinoma, squamous cell carcinoma, cervix, vagina, p53 mutations
CLINICAL IMPLEMENTATION AND OUTCOME ASSESSMENT OF DPYD PHARMACOGENOMIC TESTING TO GUIDE FLUOROPYRIMIDINES DOSING FOR CANCER PATIENTS IN SASKATCHEWAN
Dan Zhang (Department of Pathology and Laboratory Medicine, University of Saskatchewan, College of Medicine, Saskatoon, SK, Canada), Song Lu (Department of Pathology and Laboratory Medicine, University of Saskatchewan, College of Medicine, Saskatoon, SK, Canada; Saskatchewan Health Authority, Saskatoon, SK, Canada), Pramath Kakodkar (Department of Pathology and Laboratory Medicine, University of Saskatchewan, College of Medicine, Saskatoon, SK, Canada), Fergall Magee (Department of Pathology and Laboratory Medicine, University of Saskatchewan, College of Medicine, Saskatoon, SK, Canada), Haji Chalchal (Department of Oncology, University of Saskatchewan; Saskatchewan Cancer Agency, Saskatoon, SK, Canada), Vijayananda Kundapur (Department of Oncology, University of Saskatchewan; Saskatchewan Cancer Agency, Saskatoon, SK, Canada), Yanwei Xi (Department of Pathology and Laboratory Medicine, University of Saskatchewan, College of Medicine, Saskatoon, SK, Canada; Saskatchewan Health Authority, Saskatoon, SK, Canada), Fang Wu (Department of Pathology and Laboratory Medicine, University of Saskatchewan, College of Medicine, Saskatoon, SK, Canada; Saskatchewan Health Authority, Saskatoon, SK, Canada)
Objective: 5-Fluorouracil (5-FU) and its prodrug Capecitabine are commonly used chemotherapy agents for solid tumours, including colorectal, breast, and gastrointestinal cancers. However, 10-30% of patients experience severe toxicity, and 0.5-1% develop life-threatening complications, primarily due to Dihydropyrimidine Dehydrogenase (DPD) deficiency, the enzyme responsible for 5-FU metabolism. Variants in the DPYD gene reduce or eliminate DPD activity, significantly increasing the risk of toxicity. DPYD genotyping enables early identification of patients at risk, allowing for dose adjustments that improve treatment safety. This study validated and implemented DPYD genotyping in Saskatchewan cancer patients and assessed clinical outcomes post-implementation.
Methods: Six DPYD variants associated with DPD deficiency, as recommended by the 2017 Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines, were analyzed using the Elucigene DPYD genotyping kit (Yourgene Health, UK). The assay was validated following American College of Medical Genetics and Genomics standards to ensure 100% sensitivity, specificity, accuracy, and reproducibility. Over six months, 301 patient samples were tested. Eight months post-implementation, patient demographics, treatment regimens, dose adjustments, and toxicity incidence were retrospectively evaluated.
Results: The assay demonstrated high precision with a detection limit of 1.25 ng/µL DNA. Among 301 patients, 22 (7.3%) carried at least one DPYD variant, most frequently HapB3 heterozygous (5.9%). 21 enzyme-deficient patients received dose adjustments, leading to improved chemotherapy tolerance and reduced toxicity rates.
Conclusion: DPYD genotyping enables personalized fluoropyrimidine dosing, significantly reducing severe toxicity risk. This study supports the integration of pharmacogenomic testing into oncology to enhance treatment safety, efficacy, and precision medicine in cancer care.
Keywords: DPYD Genotyping, Fluoropyrimidine Toxicity, Personalized Medicine, Chemotherapy Safety
CONGENITAL DIARRHEA: A REVIEW OF 43 SMALL INTESTINAL BIOPSIES, DIAGNOSTIC APPROACHES, PITFALLS IN INTERPRETATION AND LITERATURE REVIEW
Maryam Monajemzadeh (Pathologist, Department of Pathology and Molecular Medicine, McMaster University, Hamilton, ON, Canada), Ali Zahedi (Pathologist, Department of Pathology, Tehran University of Medical Sciences, Tehran, Iran), Fatemeh Farahmand (Pediatric gastroenterologist, Tehran University of Medical Sciences, Tehran, Iran), Reza Khorvash (Arizona College of Osteopathic Medicine, Midwestern University, Glendale, Arizona, USA), Mania Mozaffari (Pathologist, Department of Pathology, Tehran University of Medical Sciences, Tehran, Iran)
Congenital enteropathy (CE) is defined as diarrhea lasting more than 2 weeks in infants for which infectious causes have been excluded. There are increasingly well-characterized infantile enteropathies that were previously called idiopathic. However, multiple conditions can be diagnosed using special tests, electron microscopy and genetic evaluation. CEs have a broad spectrum of differential diagnoses, including genetic defects, inflammation, allergies, structural gut abnormalities, and idiopathic causes. Small intestinal biopsy is a significant component of the diagnostic workup for patients with infantile diarrhea. Although a definitive diagnosis is often difficult or impossible based solely on the light microscopic examination of duodenal biopsies, it provides valuable information. In addition, the inflammatory activity and pattern of inflammatory cell infiltration can discriminate between some disorders, such as hypersensitivity reactions. In this case series, we reviewed the small bowel biopsies of 43 infants with congenital diarrhea with unclear causes. In addition to routine evaluation using H&E, we stained the biopsies for CD10 and PAS, EPCAM, and chromogranin to identify cases with microvillous inclusion disease, tufting enteropathy, and enteroendocrine cell dysgenesis, respectively. Routine HE shows a spectrum of minimal architectural changes to severe villous flattening with or without Crypt hyperplasia. Two patients exhibited an absence of endocrine cells, suggesting enteroendocrine cell dysgenesis, whereas other cases displayed a regular pattern of staining with chromogranin, EpCAM, CD10, and PAS. Four cases showed marked eosinophil infiltration, suggestive of a hypersensitivity or allergic reaction. In further follow-ups, one case with normal CD10 and PAS staining was found to have microvillous inclusion disease using electron microscopy on another biopsy specimen in a different center. In conclusion, the routine use of an IHC panel consisting of chromogranin, CD10, and EpCAM is recommended in patients with congenital diarrhea, as CEs may be inapparent and subtle on routine stains or have a patchy distribution.
Keywords: Congenital enteropathy, Small intestinal biopsy, Immunohistochemistry (IHC), Microvillous inclusion disease, Enteroendocrine cell dysgenesis
DESIGN AND VALIDATION OF A SINGLE-BLADE DEVICE FOR REPEATABLE PROSTATE SPECIMEN SECTIONING
Vedanth Desaigoudar (School of Biomedical Engineering, University of British Columbia, Vancouver, BC, Canada), Reid Vassallo (School of Biomedical Engineering, University of British Columbia, Vancouver, BC, Canada), Pushwant S. Mattu (Department of Pathology and Laboratory Medicine, Vancouver General Hospital, Vancouver, BC, Canada), Takeshi Namekawa (Department of Urologic Sciences, University of British Columbia, Vancouver, BC, Canada), Miles Mannas (Department of Urologic Sciences, University of British Columbia, Vancouver, BC, Canada), Peter C. Black (Department of Urologic Sciences, University of British Columbia, Vancouver, BC, Canada), Septimiu E. Salcudean (School of Biomedical Engineering, University of British Columbia, Vancouver, BC, Canada; Department of Urologic Sciences, University of British Columbia, Vancouver, BC, Canada; Department of Electrical and Computer Engineering, University of British Columbia, Vancouver, BC, Canada), Ersaic C. Belanger (Department of Pathology and Laboratory Medicine, Vancouver General Hospital, Vancouver, BC, Canada; Department of Pathology and Laboratory Medicine, University of British Columbia, Vancouver, BC, Canada)
Objective: To design and validate a universal prostate specimen sectioning device that is user-safe, immobilizes the tissue during sectioning, and acquires parallel sections of uniform thickness (mean of 3.5 mm) for prostates of varying dimensions.
Methods: The device was designed using computer-aided design software and 3D printed using polylactic acid filament with a fused deposition modelling 3D printer. Four surgically removed prostates were sectioned following overnight formalin fixation. The seminal vesicles, apex, and bladder neck were first removed using a scalpel. The specimen was placed in the device, immobilized, and sectioned consecutively along the superior-inferior axis using a single feather-trimming blade. Thickness was measured at the center of each section using a digital caliper (accuracy of ± 0.2 mm).
Data and Results: Figure 1 illustrates device performance. Total material cost was $40. We generated 33 sections across four specimens, with a mean section thickness of 3.4 ± 0.5 mm. Prostate size ranged from 3.2 to 4.3 cm across the superior-inferior axis.
Conclusions: Our device serves as an accurate, low-cost, and safe method to section prostates. Consistent section thickness may improve pathological stage determination and can be used to compare to preoperative imaging.
Keywords: Prostate, sectioning, computer-aided design
DESQUAMATIVE INTERSTITIAL PNEUMONIA: A RETROSPECTIVE HISTOPATHOLOGICAL STUDY EMPHASIZING KEY MORPHOLOGICAL FEATURES FOR ACCURATE DIAGNOSIS: A DESCRIPTIVE REVIEW
Rumman Ahmed
Objective: Desquamative interstitial pneumonia (DIP) is a rare smoking-related interstitial lung disease characterized histologically by diffuse intra-alveolar macrophage accumulation. This study outlines diagnostic challenges and emphasizes key histopathological and immunohistochemical features essential for accurate diagnosis and differentiation from related interstitial pneumonias.
Design/Methods: A retrospective review of biopsy-confirmed DIP cases (2010–2023) across three academic centers was performed. Clinical presentation, imaging, pulmonary function testing, histopathology, and staining results were reviewed. Diagnosis was based on consensus histologic criteria with clinicoradiologic correlation.
Results: 118 patients (mean age 52; 89% smokers) were identified. High-resolution CT scans commonly revealed bilateral ground-glass opacities with small cystic airspaces, corresponding histologically to dilated alveolar ducts and early bronchiectasis. Pulmonary function tests demonstrated restrictive physiology with decreased DLCO.
Histopathological analysis showed diffuse, uniform accumulation of intra-alveolar pigmented macrophages with eosinophilic cytoplasm—termed “smoker’s macrophages.” Pigment was light brown, non-hemosiderin (Prussian blue–negative), and PAS-positive. Marijuana-associated cases showed finer golden-brown particles. CD68 immunostaining confirmed macrophage identity. Alveolar septa showed mild chronic inflammation, lymphoid aggregates, eosinophils, and occasional multinucleated giant cells. Architecture was largely preserved, with mild interstitial fibrosis; fibroblastic foci were absent.
Differential diagnosis included RB-ILD (bronchiolocentric macrophage accumulation with less inflammation), NSIP (interstitial fibrosis without smoker’s macrophages), and PLCH (Langerhans cell nodules, S100/CD1a-positive). BAL findings were non-specific but often macrophage-predominant.
Conclusion: DIP diagnosis requires surgical lung biopsy due to non-specific clinical and radiologic findings. Recognition of diffuse alveolar macrophage infiltration, PAS-positive pigment, Prussian blue negativity, and lack of fibroblastic foci are key to distinguishing DIP from other smoking-related ILDs. Accurate pathological assessment using histology and immunostains is essential for diagnosis and management.
Keywords: Pneumonia, smoking, macrophage, fibrosis, interstitial
DIGITAL ALTERNATIVES TO THE TEACHING AUTOPSY
Ciara Perez, MD BSC, CBME
Background: The teaching autopsy was a cornerstone of medical education for centuries, and yet few medical students today will have had the opportunity to observe one. Unlike cadaveric dissection, an educational exercise, an autopsy is a post-mortem examination conducted by physicians to determine cause of death and understand the pathophysiology of disease. Logistical and ethical challenges have contributed to a decline in the use of autopsies for medical education in recent years; however, evidence suggests that observing an autopsy offers significant educational value, including in the areas of ethics and the socioemotional “hidden curriculum” of medicine. This study explores the potential application of digital pathology tools to replace traditional teaching autopsies in undergraduate medical education.
Methods: A review of the literature was conducted using Medical Subject Headings (MeSH) and keywords to identify relevant publications in Ovid MEDLINE and Web of Science. Peer-reviewed research and educational materials are included in the search. Data was extracted with particular attention to the technologies used, educational outcomes, and ethical and logistical considerations.
Results: Digital tools are increasingly utilized in medical education and have the potential to simulate autopsy learning. Advanced imaging techniques, such as 3D reconstruction, allow students to interact with anatomy, although they cannot replicate the sensory aspects offered by an in-person autopsy. Augmented and virtual reality offer a promising immersive, real-world experience but remain in the experimental stages. Case-based learning using digital pathology and telecommunication have been used in anatomical pathology residency programs, though the effectiveness and broader ethical implications of these approaches remain unclear.
Conclusions: Further research is needed to determine the effectiveness of these digital tools in achieving comparable learning outcomes to the teaching autopsy, especially with regard to the psychosocial impact. However, the integration of these technologies could allow more medical students to have access to the teaching autopsy.
Keywords: Digital pathology, autopsy, medical education
DIGITAL PATHOLOGY BEYOND SURGICAL PATHOLOGY: TAILORED APPROACHES FOR HEMATOPATHOLOGY, CYTOPATHOLOGY, AND MEDICAL MICROBIOLOGY
Mark Tubingan (Department of Laboratory Medicine & Pathology, University Health Network, Toronto, ON, Canada), Vasudha Raghunathan (Engineering & Operations, Pramana Inc, Toronto, ON, Canada), Bharathwaj Raghunathan (Engineering, Pramana Inc, Toronto, ON, Canada), Carlo Vincent Hojilla (Department of Laboratory Medicine & Pathology, University Health Network, Toronto, ON, Canada)
Objective: The objective of this study is to evaluate the unique digital pathology requirements of hematopathology, cytopathology, and medical microbiology. The aim is to develop evidence-based strategies that address critical variables, including magnification, z-stacking, and color profile optimizations. By tailoring digital approaches, this work seeks to inform a comprehensive strategy for digital pathology implementation for these subspecialties.
Design/Methods: A pilot study analyzed selected peripheral blood smears, bone marrow aspirates and cytology slides (Romanowsky-based, Prussian Blue, alcohol-based slides). Whole slide images were acquired at 40X and 80X using the Pramana Spectral HT2 scanner. Z-stack configurations were tested, and color fidelity was assessed using specific colour profiles.
Results: Using a standardized scan area, scan durations increased 3.8-fold at 80X magnification compared to 40X. This magnification-dependent effect was more pronounced in bone marrow aspirates than in peripheral blood smears. Scan times also correlated with z-stack quantity, though the relationship differed by specimen type: peripheral blood smears showed no significant differences in scan time across 7, 11, or 13 z-stacks, while marrow aspirates exhibited progressively longer scan times with increasing z-stack layers. Reducing z-stack numbers reduced scan time by 27.1% for marrow aspirates but only 3.4% for peripheral blood smears. Custom color profiles optimized for individual specialized stains significantly improved diagnostic concordance.
Conclusions: Our preliminary study demonstrates that subspecialties require tailored digital approaches distinct from surgical pathology. Higher magnifications, optimized z-stacking parameters, and specialized color profiles are essential for diagnostic accuracy but significantly impact image acquisition. A one-size-fits-all approach to digital pathology implementation is inadequate. We propose a pan-Canadian framework for digital pathology that acknowledges subspecialty-specific requirements, establishes standardized scanning protocols for different specimen types, and incorporates standardized color profiles for specialized stains. Further multi-institutional validation studies are needed to refine these parameters and develop consensus guidelines for comprehensive digital pathology implementation.
Keywords: Digital Pathology, Z-Stack, Hematopathology, Cytopathology, Medical Microbiology
ER STATUS MIGRATION IN NSMP ENDOMETRIAL CANCERS: COMPARING A 10% AND 1% THRESHOLD FOR POSITIVITY
Ashlyn Fong (Department of Pathology, University of Colorado Anschutz Medical Campus, Aurora CO, USA), Kurtis Davies (Department of Pathology, University of Colorado Anschutz Medical Campus, Aurora CO, USA), Rebecca J. Wolsky (Department of Pathology, University of Colorado Anschutz Medical Campus, Aurora CO, USA)
Background: ER status may further stratify NSMP endometrial carcinomas (EC), with ER negativity (ERnNSMP) portending a worse prognosis. In clinical practice, it is common to define ER positivity as >1% of tumour cells. Vermij et al (PMID: 36690721) recently found a threshold of 10% holds more discriminative power. This study aims to define ER status migration, comparing the 1% and 10% thresholds, and to describe ERnNSMP cases.
Design: Consecutive EC resections at a single tertiary care center (2022-2025) underwent TCGA/ProMisE classification (POLE by NGS panel; MMR, p53 by IHC) and IHC for ER (SP1, Ventana): clinically scored as ER+ if > 1% expression, then reclassified using > 10%. Histotype, TCGA/ProMisE classification, FIGO grade/stage, and lymphovascular invasion (LVI) were evaluated. For ERnNSMP, clinical outcomes were also examined. Pearson Chi-square statistical analysis was performed, (p< 0.05 considered significant).
Results: Of 478 EC, 205 (42.9%) were NSMP. Of those, 8 (3.9%) were ER negative using the 1% threshold. Applying a 10% cut-off increased the number to 15 (7%). Of the ERnNSMP, 4/15 (27%) had short interval recurrence/metastases and extensive LVI; these cases were FIGO stage IB, IIIA and IVB. See Table 1.
NSMP EC, with ER positivity (ERpNSMP) enrich for APC, AR, ARID1A, ATM, BRCA2, CDH1, CTNNB1, DICER1, FAT3, KMT2C, KRAS, MET, PIK3CA, POLD1, PTEN and ROS1 mutations compared to other TCGA/ProMisE categories (p < 0.05). ERnNSMP does not appear to enrich for specific gene mutations.
Conclusion: A 10% threshold for ER positivity may significantly increase the number of ERnNSMP EC, impacting therapeutic approaches. The majority of ERpNSMP are endometrioid carcinomas, enriched for mutations common to this histotype. The impact of ER expression on risk stratification in ERnNSMP warrants further investigation.
Keywords: Endometrial cancer, ER IHC, Risk stratification, TCGA/ProMisE
EVALUATING THE UTILITY OF ADDITIONAL SAMPLING ON GALLBLADDER WITH INCIDENTAL HISTOPATHOLOGY FINDINGS
Pei Yu (Laboratory Medicine and Pathobiology, University of Toronto, Toronto, Ontario, Canada), Lina Chen (Laboratory Medicine and Pathobiology, University of Toronto, Toronto, Ontario, Canada; Sunnybrook Health Sciences Centre, Toronto, Canada; Anatomic Pathology, Sunnybrook Health Sciences Centre, Toronto, Canada)
Objective: Cholecystectomy specimens may reveal incidental findings. Taking extensive additional sections or submitting the gallbladder entirely for certain incidental findings such as atypia and dysplasia is the routine practice. However, the necessity of extensive histological sampling remains uncertain. This study aims to evaluate whether additional sampling influences the final diagnosis on incidental findings of cholecystectomies.
Methods: A retrospective review was conducted on the gallbladder specimens resubmitted for additional sections over a 10-year period at Sunnybrook Health Sciences Centre. Data extraction included patient demographics, clinical presentation, macroscopic findings, number of initial and additional sections submitted, and final histopathological diagnoses. The initially submitted slides were retrieved and reviewed to assess the rationale for additional sampling, and final diagnoses were compared with initial findings to determine any diagnostic changes.
Results: A total of 49 cholecystectomy cases were analyzed. On average, 2 sections were initially submitted per case. Following initial diagnosis, 30 cases underwent total submission of the remaining tissue, while 19 cases had selective additional sampling, with an average of 7 extra sections submitted per case. Initial diagnoses included: no mucosa identified (N=3), intracystic papillary neoplasm (ICPN, N=2), reactive changes (N=22), low-grade dysplasia (N=12), high-grade dysplasia (N=4), and malignancy (N=6, including invasive carcinoma and neuroendocrine tumours). Only one case (1/49, 2%) of low-grade dysplasia was upgraded to high-grade dysplasia after additional section submission, while all other cases retained their initial diagnosis.
Conclusion: Extensive additional sampling rarely alters the diagnosis of incidental gallbladder findings. In the absence of gross abnormalities, incidental atypia or dysplasia carries no hidden risk of invasive carcinoma.
Keywords: Gallbladder, dysplasia, additional sampling, diagnostic upgrade
EVALUATION OF HIPPO PATHWAY PROTEIN AND MRNA EXPRESSION IN HUMAN FETAL LUNGS AFFECTED BY CONGENITAL DIAPHRAGMATIC HERNIA
Claire Cheung (Department of Pathology and Laboratory Medicine, University of British Columbia), Rachel Witt (Biochemistry and Microbiology, Faculty of Science, University of Victoria), Martin A. Prusinkiewicz (Department of Pathology and Laboratory Medicine, University of British Columbia), Martina Mudri (Department of Surgery, Faculty of Medicine, University of British Columbia), Mariya I. Goncheva (Biochemistry and Microbiology, Faculty of Science, University of Victoria), Anna F. Lee (Department of Pathology and Laboratory Medicine, University of British Columbia)
Objective: Congenital diaphragmatic hernia (CDH) arises from incomplete diaphragm development in the fetal period, leading to abdominal organs herniating into the thorax, and lung hypoplasia which complicates postnatal hernia repair. Mechanical compression of developing lungs, and altered molecular pathways of lung development such as Hippo, are involved in CDH lung hypoplasia. Animal studies suggest a role for Hippo in CDH pathogenesis through its main effector, YAP, but human studies are lacking. We hypothesize that Hippo pathway gene/protein expression is altered in human CDH lungs.
Design/Methods: Fetal autopsy formalin-fixed, paraffin-embedded (FFPE) lung sections from 10 CDH cases (bilateral; 17-28 weeks’ gestational age (wga)) and 5 non-CDH controls (left lung only; 18-36 wga) were immunostained with anti-YAP. Positive (cytoplasmic and/or nuclear) staining was expressed as a percentage of total cells counted/slide, with epithelial and interstitial cells counted separately. Quantitative PCR (qPCR) of RNA samples extracted from FFPE of 11 CDH lungs and 7 control lungs was performed on Hippo pathway candidate genes TAZ, TEAD1, TEAD2, TEAD3, TEAD4, and LATS2, and normalized to beta-actin.
Results: Both CDH and control lungs showed significantly decreased YAP expression in the epithelium with increasing gestational age (p=0.0025), but not in the interstitium (p=0.0593), leading to a significant decrease in overall (interstitium plus epithelium) YAP protein expression with increasing gestational age (p=0.0105). There was no significant difference in YAP expression between CDH and control lungs. qPCR found very low-level target gene expression in all tested samples.
Conclusion: Our results suggest that YAP protein expression in human fetal lung decreases with advancing fetal gestational age, but CDH does not appear to play a major role in influencing YAP expression during fetal development. A more sensitive approach than conventional qPCR may be needed to detect any differences in Hippo pathway gene expression between human CDH and control lungs.
Keywords: Congenital diaphragmatic hernia, Hippo, fetus, autopsy, lungs
GLIOMAS WITH IMMUNOHISTOCHEMICAL LOSS OF MMR PROTEINS: A SPECTRUM OF LYNCH SYNDROME AND CMMRD: CLINICO-PATHOLOGICAL EVALUATION, A TERTIARY CARE CANCER INSTITUTE EXPERIENCE
Caroline Thomson (Departments of Pathology), Neelam Bhandari (Departments of Pathology), Ramandeep Arora (Departments of Pathology), Ayushi Sahay (Departments of Pathology), Aekta Shah (Departments of Pathology), Tejpal Gupta (Radiation Oncology), Maya Prasad (Pediatric Oncology), Girish Chinnaswamy (Pediatric Oncology), Sridhar Epari (Departments of Pathology)
Rationale: Mismatch repair (MMR) deficiency in high-grade gliomas (HGG) can be sporadic or mono-allelic (Lynch syndrome) and bi-allelic (CMMRD) germline mutations of MMR genes.
Objective: Evaluate the clinico-pathological features of MMR-immunodeficient/altered HGG.
Material and Methods: Forty-four cases of histologically HGG with no IDH and H3 mutations that showed immunohistochemical loss of MMR proteins formed the study-cohort.
Results: Pattern 1 (loss in both tumour and native cells, n=27): Median age: 8 years (4-33); 3 patients >18 years. Male:female ratio: 1.45:1. Cerebrum (n=24) was the commonest site. Café au lait macules (CALM, n=20), consanguinity (CS) (n=12), family history of malignancy (FHM) (n=11), and other malignancies (n=5) were reported. Histology showed bizarre giant cells (n=18) and undifferentiated morphology (n=10). p53 immunopositivity was seen in 23 cases, with ATRX loss in 13. Combined MLH1 & PMS2 loss (n=11), isolated PMS2 loss (n=11); combined MSH2 and MSH6 loss (n=1), isolated MSH2 loss (n=1) and isolated MSH6 loss (n=2) were observed.
Pattern 2 (loss in tumour cells only, n=17): Median age: 31 years (8-70); 14 patients >18 years. Male:female ratio: 2.4:1. Cerebrum (n=13) was the most frequent location. CALM (n=1), FHM (n=4), and other malignancies (n=4) were noted. p53 positivity was observed in all cases, with ATRX retention in 8. MSH6 loss was common (n=7) alongside MSH2 & MSH6 loss (n=7).
Conclusion: CMMRD cases are often in paediatric-age and show combined MLH1 & PMS2 loss and isolated PMS2 loss, while Lynch syndrome is characterized by combined MSH2 & MSH6 loss and isolated MSH6 loss.
Keywords: Mismatch cancer syndrome, High grade glioma, MMR, immunohistochemistry
MESONEPHRIC LIKE ADENOCARCINOMA OF THE ENDOMETRIUM: A POTENTIAL DIAGNOSTIC PITFALL AND INSTITUTIONAL EXPERIENCE
Gawa Bidla (Department of Pathology and Molecular Medicine, McMaster University Medical Centre, Hamilton, Ontario; Department of Pathology and Molecular Medicine, Juravinski Hospital and Cancer Centre, Hamilton, Ontario), Andra Nica (Department of Oncology, Division of Gynecologic Oncology, Juravinski Hospital and Cancer Centre, Hamilton, Ontario), Odette Boutross-Tadross (Department of Pathology and Molecular Medicine, McMaster University Medical Centre, Hamilton, Ontario), Monalisa Sur (Department of Pathology and Molecular Medicine, Juravinski Hospital and Cancer Centre, Hamilton, Ontario; Department of Oncology, Division of Gynecologic Oncology, Juravinski Hospital and Cancer Centre, Hamilton, Ontario)
Background: Mesonephric-like adenocarcinoma (MLA) of the female genital tract is a recently described rare adenocarcinoma of the uterine corpus and ovary. This subtype can be very challenging to diagnose as it can mimic other endometrial carcinomas (EC) particularly low grade endometrioid adenocarcinoma (ECa). MLA often present at advanced stage with frequent recurrence and distant metastasis. Misdiagnosis of MLA may prevent the patient from benefiting from treatment that is reserved for more aggressive EC. Post hysterectomy, these patients receive radiation only (stage 1 or 2) or a combination of chemotherapy and radiation (stage 3 or 4).
Design: All diagnoses of MLA and EC that were negative for ER/PR accessioned to our medical record in last 3 years were reviewed. TTF-1 and GATA-3 immunohistochemical (IHC) stains, and next generation sequencing (NGS) was additionally performed on FFPE tissue on all cases using Roche Kit for endometrial biomarkers and Thermofisher Scientific system.
Result: A total of 8 MLA cases including 2 metastatic cases were analyzed. Age ranged from 42-82 years. 2 cases recurred sites included pelvis, omentum, brain, lung and liver. A combination of histologic features, immunohistochemistry (ER/PR negative with GATA-3/TTF-1 reverse staining pattern) and molecular profile with KRAS mutation led to the accurate diagnosis of MLA (table 1).
Conclusion: MLA diagnosis on morphology is challenging as it can mimic wide range of histologic patterns including endometroid, mucinous, serous and clear cell carcinoma. Some MLA can have a background of atypical hyperplasia or endometriosis similar to ECa. A combination of morphology, IHC and molecular testing is invaluable in arriving at the diagnosis of MLA. Clues that may lead to further characterization include but are not limited to glomerular-like, tubular, villous morphology with bland cytology and brisk mitosis, ER/PR tumour negativity, TTF-1/GATA-3 reverse positivity and KRAS mutation.
Keywords: Mesonephric-like adenocarcinoma, endometrial carcinoma
METHYLATION-BASED DROPLET DIGITAL PCRS FOR THE DIAGNOSIS OF INTRAHEPATIC CHOLANGIOCARCINOMA
Daniel Xia (Laboratory Medicine Program, University Health Network), Natalie Boruvka (Advanced Molecular Diagnostics Laboratory, University Health Network), Tong Zhang (Advanced Molecular Diagnostics Laboratory, University Health Network), Harriet Feilotter (Advanced Molecular Diagnostics Laboratory, University Health Network), Kai Duan (Laboratory Medicine Program, University Health Network)
Objective: Intrahepatic cholangiocarcinoma (iCCA) is the second most common primary liver cancer; yet, its diagnosis poses significant challenges due to the absence of specific diagnostic markers. We aim to develop simple and inexpensive methylation-based droplet digital PCRs to be used as potential diagnostic markers for iCCA in clinical practice.
Design/Methods: The Cancer Genome Atlas (TCGA) network methylation array data was analyzed to identify highly informative CpG sites that are differentially methylated between cholangiocarcinomas (CHOL), normal liver, and tumours that mimic CHOL on histopathology (pancreatic and gastric adenocarcinomas, amongst others). Two PCRs, using methylation-independent primers and methylation-dependent probes, were developed to assess 2 such CpG sites. To date, the 2 PCRs have been tested on formalin-fixed paraffin-embedded (FFPE) samples of small duct iCCA, large duct iCCA and distal extrahepatic CHOL from our institution.
Results: Two PCRs developed correspond to array probes cg07351675 (probe 1) and cg27146152 (probe 2). We defined a metric as the numeric difference in methylation beta-values between the two probes (i.e., probe 1 minus probe 2) and found that this TCGA array metric can accurately distinguish CHOL (red and orange) from normal liver (yellow), hepatocellular carcinoma (LIHC), colorectal (CORE), gastric/esophageal (GEAD), and pancreatic adenocarcinomas (PAAD; all white; see Fig. 1). The best separation was observed for molecular subtypes correlated with small duct iCCA (IDH, METH2, and METH3 TCGA clusters; red). On testing using internal FFPE samples, the corresponding PCR metric (PCR 1 minus PCR 2) separated small duct from large duct iCCA and distal extrahepatic CHOL (Fig. 2).
Conclusions: The 2 PCRs show promise as diagnostic markers for iCCA, particular small duct type iCCA, which are known to correlate with actionable genetic alterations such as FGFR2 fusions and IDH mutations. Testing on gastric and pancreatic liver metastases is in progress.
Keywords: Cholangiocarcinoma, methylation, PCR, small duct, intrahepatic
MULTIPLE-CLASSIFIER ENDOMETRIAL CANCERS: A PROSPECTIVE STUDY OF CLINICOPATHOLOGICAL CHARACTERISTICS AND PROGNOSTIC FACTORS
Sameh Youssef (Pathology and Molecular Medicine, Juravinski Cancer Center and Hospital, McMaster University), Daria Grafodatskaya (Pathology and Molecular Medicine, Juravinski Cancer Center and Hospital, McMaster University), Maria Vladoiu (Pathology and Molecular Medicine, Juravinski Cancer Center and Hospital, McMaster University), Andra Nica (Department of Oncology, Gynecology Oncology Division, Juravinski Cancer Center, McMaster University), Alice Lytwyn (Pathology and Molecular Medicine, Juravinski Cancer Center and Hospital, McMaster University), Monalisa Sur (Pathology and Molecular Medicine, Juravinski Cancer Center and Hospital, McMaster University)
Background: Endometrial cancer (EC) has been categorized into 4 molecular subtypes: POLE-ultramutated (POLEmut), mismatch repair-deficient (MMRd), no specific molecular profile (NSMP), and p53-abnormal (p53abn). These subtypes guide prognosis and treatment. Tumours with more than one molecular feature (POLEmut-MMRd, (POLEmut-p53abn) and (MMRd-p53abn), termed “multiple classifiers,” pose challenges in classification and management particularly when conflicting molecular features favor opposing treatment strategies.
Objective and Methods: Our objective was to investigate clinicopathological, p53 IHC staining patterns and prognostic factors associated with multiple classifiers. Cases with multiple classifiers reported in 2024 at Juravinksi Hospital were identified at the time of sign out. MMR and p53 were assessed by immunohistochemistry, TP53 and POLE mutation by next-generation sequencing (NGS). Results. 20 cases were identified as multiple classifiers. Mean patient age ranged from 62-88 yrs. See Table 1. Among the 9 POLE mutant cases, 8 demonstrated subclonal p53 mutant pattern.
Conclusions: The multiple classifiers with POLE mutation appear to share favorable prognostic factors, often associated with lower stage, lower-grade histology, and fewer cases of lymphovascular invasion compared to MMRd-p53abn. Further research and long-term follow-up are needed to understand the correlation between the histological prognostic factors and the molecular classifications in predicting clinical outcomes.
Keywords: Endometrial cancer, Multiple classifiers, POLE, Molecular classification
ONE YEAR OF ULTRA-RAPID MOLECULAR TESTING THROUGH THE IDYLLA PLATFORM DEMONSTRATES IMPROVED PATIENT CARE OUTCOMES COUPLED WITH A MARKEDLY REDUCED TURNAROUND TIME
Katherina Baranova (Department of Pathology and Laboratory Medicine, London Health Sciences Center, London, ON, Canada), Laura Lockau (Department of Pathology and Laboratory Medicine, London Health Sciences Center, London, ON, Canada), Louise Mui (Department of Pathology and Laboratory Medicine, London Health Sciences Center, London, ON, Canada), Elissa Woo (Department of Pathology and Laboratory Medicine, London Health Sciences Center, London, ON, Canada), Matthew Cecchini (Department of Pathology and Laboratory Medicine, London Health Sciences Center, London, ON, Canada)
Introduction: The Idylla platform (Biocartis) is a fully automated, real-time polymerase chain reaction (PCR)-based molecular testing system which reports results in 3 hours. The Idylla platform was introduced at London Health Sciences Center (LHSC) in January 2024 with a total of over one year of testing experience to date.
Methods: We describe our implementation of this system for testing of BRAF, EGFR, and KRAS on clinician request, using formalin-fixed, paraffin-embedded surgical and cytology cell block samples as part of a quality assurance study. All patient samples in this study were subsequently tested using laboratory-developed next generation sequencing (NGS)-based assays. Chart review was performed for each case with an actionable result to determine the clinical impact.
Results: 55 cases underwent molecular testing through Idylla with an average turnaround time of one day from clinician request to reporting of results. The turnaround time was shortened by 16 days on average. Cases included lung adenocarcinoma, anaplastic thyroid carcinoma, colorectal adenocarcinoma, and carcinomas of unknown primary. Cytology specimens (n=18) and surgical specimens (n=37) were both tested successfully. Of these 24 found an actionable mutation, 15 in EGFR, 4 in KRAS, and 5 in BRAF. There was excellent concordance with follow-up testing by NGS. There was one indeterminate result and one sample with insufficient material for testing. There were no demonstrated false negatives or false positives. Review of each case demonstrated a number of positive outcomes, including utilization of targeted therapy rather than whole brain radiation, and more rapid start times to therapy. In several cases, patients were acutely ill from their underlying disease and rapid testing was critical to making the best treatment decisions. Clinician feedback was uniformly positive.
Discussion: The Idylla platform is an accessible, rapid, and reliable testing option with demonstrated benefit following implementation at LHSC.
Keywords: Molecular pathology, quality assurance, targeted therapy
PAGETOID SPREAD OF BASAL CELL CARCINOMA - A CASE SERIES
Tyler Wong (Max Rady College of Medicine, University of Manitoba, Winnipeg, MB), Sate Hamza (Department of Pathology, University of Manitoba, Winnipeg, MB; Shared Health, Winnipeg, MB), Marc Ranson (Department of Pathology, University of Manitoba, Winnipeg, MB; Shared Health, Winnipeg, MB)
Introduction: Pagetoid spread of basal cell carcinoma (BCC) is a minimally documented phenomenon. It has been described in one small case series and only briefly mentioned elsewhere. We present three cases of BCCs with pagetoid spread to increase awareness of this histological variation. This feature creates the potential for misdiagnosis, and in one of our cases did lead to an incorrect preliminary diagnosis.
Case Series: Case 1 is a 50-year-old male that presented with a right shoulder lesion which was sampled by shave biopsy. It demonstrated superficial BCC, with patchy pagetoid scatter of carcinoma cells. Case 2 is a 48-year-old female that presented with a lesion on the chest that was excised. It demonstrated a clear cell nodular BCC, and showed pagetoid scatter of carcinoma cells with clear cytoplasm. Case 3 is a 62-year-old male that presented with a patch to the right thigh which was sampled by punch biopsy. It showed histologically subtle superficial BCC with pagetoid scatter of individual and small nests of carcinoma cells. A preliminary diagnosis of melanoma in situ was rendered. Dermatopathology consultation and additional studies revealed the lesion to be a BCC.
Conclusions: The presence of pagetoid carcinoma cells is not typically associated with BCC, and may be misleading in the consideration of differential diagnosis. Familiarity with this histologic variation can help prevent misdiagnosis. Case 3 of this series substantiates the potential for misdiagnosis if the salient features are not recognized.
Keywords: Pagetoid basal cell carcinoma, clear cell basal cell carcinoma, basal cell carcinoma
PILOT STUDY: COMPUTER ASSISTED PD-L1 SCORING FOR NON-SMALL CELL LUNG CARCINOMA USING OPEN-SOURCE SOFTWARE QUPATH
Pramath Kakodkar (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Daniel Markewich (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Henry Pan (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Anil Parwani (Department of Anatomical Pathology, Ohio State University, Ohio, USA), Deepti Ravi (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada)
Background: The rapid expansion in the utilization of digital pathology has the potential to streamline practice and research in anatomic pathology. QuPath is an open-source pathology software that offers reproducibility in morphometric and computer-assisted image analyses. We aimed to present this pilot study as proof-of-concept of the technical concordance of QuPath assisted PD-L1 scoring with the manual scores of 4 pathologists in Non-Small Cell Lung carcinomas (NSCLC).
Methods: Lung biopsies from patients (n=15) with NSCLC were stained with hematoxylin and eosin, and PD-L1 immunohistochemistry. These biopsies were scanned at 40x magnification on the Aperio Virtual Microscopy System and were imported into QuPath. A classifier for tumour cell detection, tumour-infiltrating lymphocytes, and PD-L1 scoring was trained using 20 representative images patches. PD-L1 scores were recorded for each of the 15 patients using cytoplasmic and membrane color segmentation and these scores were compared against pathologists quantitative and semiquantitative assessments.
Results: QuPath assisted PD-L1 scores showed strong positive correlation (correlation coefficient = 0.97) with the pathologists’ PD-L1 scores. This classifier performed in accordance with our comparative gold standard (average of the 4 pathologists) within the tested dataset of patients with PD-L1 scores in the ≥ 50%, 1-49%, and < 1 positivity range. The classifier model showed higher concordance for well-differentiated and moderately differentiated squamous cell carcinomas compared to cases with non-mucinous adenocarcinoma.
Conclusion: Our automated PD-L1 scoring system for NSCLC showed accuracy similar to our pathologists. The next phase of this study is to proceed to a comprehensive validation of this QuPath classifier. The utilization of our classifier with this open-source software will facilitate the integration of automated scoring into the clinical workflows.
Keywords: QuPath, Digital Pathology, TPS, PD-L1
PILOT STUDY: INNOVATIVE APPLICATION OF OPTICAL GENOME MAPPING FOR ALPHA-THALASSEMIA DIAGNOSIS
Pramath Kakodkar (Department of Pathology and Laboratory Medicine, University of Saskatchewan, Saskatoon, SK, Canada), Holly Giasson (Department of Pathology and Laboratory Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Advanced Diagnostics Research Lab, University of Saskatchewan, Saskatoon, SK, Canada), Gaby Tanumihardja (Department of Pathology and Laboratory Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Advanced Diagnostics Research Lab, University of Saskatchewan, Saskatoon, SK, Canada), Karen Mochoruk (Department of Pathology and Laboratory Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Advanced Diagnostics Research Lab, University of Saskatchewan, Saskatoon, SK, Canada), Hadi Goubran-Messiha (Department of Hematology and Oncology, Saskatchewan Cancer Agency, Saskatoon, SK, Canada), Matthew Nicholson (Department of Hematology and Oncology, Saskatchewan Cancer Agency, Saskatoon, SK, Canada), John F. DeCoteau (Department of Pathology and Laboratory Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Advanced Diagnostics Research Lab, University of Saskatchewan, Saskatoon, SK, Canada)
Background: Alpha-thalassemia (AT) is a hemoglobinopathy caused by diminished α-globin expression due to deletions in chromosome 16 α-globin gene clusters. AT was historically rare in Canada, but has been rising due to immigration from AT prevalent regions. Conventional AT detection involves hemoglobin electrophoresis, and high-performance liquid chromatography (HPLC) followed by confirmatory molecular testing. This confirmatory test is currently a send-out test resulting in a 6-week turnaround time (TAT). We propose a novel Optical Genome Mapping (OGM) assay for the rapid detection of AT.
Methodology: 12 patients with microcytosis (MCV< 81.9fl) suspected for AT by HPLC were selected. Peripheral blood samples were analyzed using OGM (Bionano Genomics Inc.). Ultra-high molecular weight genomic DNA was isolated, labeled, and analyzed on the Bionano Saphyr system. OGM data was aligned against the reference human genome (GRCh38/Hg20) to flag deletions in α-globin gene cluster.
Results: Our cohort (n=12, median: 21.5y, M:F=7:5) had an average MCV of 68.6±7.2fl and predominant HPLC result of “AT or rare forms of Beta-thalassemia (BT) cannot be ruled out” (n=3), and “repeat after iron-deficiency anemia correction” (n=3). In 2 cases, HPLC results were consistent with BT trait due to elevated HbA2 levels (6.0% and 6.6%). OGM identified five cases of presumptive AT based on homozygous or heterozygous HBA2 deletions (3.2-3.7kb) in 3 patients and cis deletion (16.5-16.7kb) of HbA2 and HBA1 in 2 patients consistent with Southeast Asian (SEA) deletion. No α-gene deletion was detected via OGM in two cases of presumptive BT trait.
Conclusion: OGM identified one and two gene deletional AT in five patients with suspected AT within a 3-day TAT. OGM is superior to conventional testing as it is unaffected by iron deficiency or transfusions. Comprehensive validation using patients with a confirmed AT by molecular analysis will follow. This is the first ever utilization of OGM for AT diagnosis.
Keywords: Alpha thalassemia, OGM, Pilot study
PRELIMINARY EVALUATION OF INITIATIVES TO INCREASE MEDICAL STUDENT INTEREST IN PATHOLOGY AND LABORATORY MEDICINE
Anthea Lafreniere (Department of Laboratory Medicine and Pathobiology, Temerty School of Medicine, University of Toronto, Toronto, Ontario), Mario Capitano (Department of Laboratory Medicine and Pathobiology, Temerty School of Medicine, University of Toronto, Toronto, Ontario)
Objective: Pathology and laboratory medicine play a critical role in health care, yet medical student exposure is limited. Many students are unaware of the field’s career opportunities and clinical relevance, leading to low engagement. This study evaluates the impact of initiatives to increase student interest in pathology and laboratory medicine.
Methods: Educational, digital marketing, and experiential interventions were introduced at the University of Toronto. Key initiatives included: (1) a laboratory medicine interest group featuring a “Case of the Month” series, (2) an annual “Pathology Summit” with interactive panels and keynote speakers, (3) a dedicated departmental website, and (4) social media and targeted email campaigns. In addition, 5) A new MAPS curriculum integrating medical imaging, anatomy, pathology, and surgery; and 6) a centralized online application process for preclerkship laboratory medicine elective experiences.
Results: Engagement was assessed through website analytics, elective applications, and Canadian Resident Matching Service (CaRMS) match results. Data showed persistent engagement in the “Case of the Month” activity (average attendance of 8.71 students over 2 years with repeat attendees), moderate website content retention (1.36 views per user), increased applications for pathology electives (from five to 25 applications over last 4 years), and a positive trend in CaRMS match results (20% to 100% match rate over last three years).
Conclusion: These multimodal interventions increased engagement in pathology. Future efforts should refine and expand these initiatives to maximize impact. Future research should implement measures to understand which interventions are most strongly driving student engagement.
Keywords: pathology, medical education, student engagement, curriculum development, residency recruitment
PRIMARY INTESTINAL LYMPHOMA INCIDENTALLY DISCOVERED IN INTESTINAL POLYPS
Sedigheh Abazari (Department of Laboratory Medicine and Pathology, Unity Health Toronto, Toronto, Ontario), Catherine Streutker (Department of Laboratory Medicine and Pathology, Saint Michael’s Hospital, University of Toronto, Toronto, Ontario), Sasan Zandi, (Department of Laboratory Medicine and Pathology, Saint Michael’s Hospital, University of Toronto, Toronto, Ontario)
Objective: The gastrointestinal (GI) tract is the most frequent extranodal site for lymphomas, comprising up to 40% of extranodal non-Hodgkin lymphomas (NHL). Primary GI lymphoma, however, is relatively rare, representing about 10-15% of all NHL cases and only 2% and 0.2% of small and large intestinal malignancies, respectively. Intestinal lymphomas may present as polypoid lesions, though its incidental discovery within intestinal polyps is uncommon. This can present diagnostic challenges, particularly in small biopsy specimens, which may show crush artifacts due to the delicate nature of lymphoid tissue.
Method: We conducted a retrospective analysis of intestinal biopsy, polypectomy, and endoscopic mucosal resections (EMR) specimens diagnosed with non-Hodgkin lymphoma (NHL) over fifteen years at Unity Health Toronto (2010-2024). We collected clinical data and reviewed selected slides with a focus on cases where primary intestinal lymphoma was incidentally discovered within intestinal polyps.
Results: A total of 65 patients were diagnosed with NHL with 37 (57%) occurring in the small intestine, 21 (32%) in the large intestine, and 6 (9%) affecting both regions. Of the 63 cases with complete workup, 16 (25%) were identified as primary intestinal lymphoma. Notably, 9 cases of primary intestinal lymphoma were incidentally found within intestinal polyps, including two rare instances of rectal marginal zone lymphoma (MZL).
Conclusion: Anatomic pathologists should remain vigilant for lymphoma in the intestinal polyps. A primary immunohistochemistry panel, including CD3, CD20, pan-keratin, and CD21, can aid in identifying cell type, lymphoepithelial lesion, and follicular dendritic meshwork architecture, helping to differentiate lymphoma in suspicious lymphoid infiltrates.
Keywords: Primary intestinal lymphoma, lymphoma in colonic polyp, incidental intestinal lymphoma
PRIMARY SMARCB1-DEFICIENT YOLK SAC TUMOUR OF THE HEAD AND NECK IN A ONE-YEAR-OLD GIRL: AN EXTREMELY RARE ENTITY, CASE REPORT AND LITERATURE REVIEW
Moeinadin Safavi, Fatemeh Rostami, Reza Khorvash
Pediatric germ cell tumours (GCTs), including yolk sac tumours (YSTs), comprise a diverse group of neoplasms that arise in both gonadal and extragonadal locations and head and neck region are among the rare places where they occur. The clinical presentation and radiological findings in head and neck GCTs may not follow the usual presentation of these tumours within gonads. This unusual location can lead to delayed or incorrect diagnosis and treatment delays. Here, we report a peculiar case of a one-year-old girl who was presented with a neck mass and high alpha-fetoprotein level that finally diagnosed with YST. This case is unique due to the exceedingly rare presentation of a YST and loss of INI1, as determined by immunohistochemistry, in the head and neck region. It emphasizes the diagnostic challenges and highlights the importance of considering this diagnosis, even in unusual locations, and underscores the need to include YSTs in the differential diagnosis of pediatric neck masses to ensure timely intervention and management. Additionally, this case is unique in that it demonstrates loss of SMARCB1/INI1 expression. The differential diagnosis includes a SWI / SNF complex-deficient sinonasal carcinoma; however, the location outside the sinonasal tract excludes this possibility, although histopathologic and immunophenotypic features overlap. Given the potential involvement of SMARCB1 in YST pathogenesis, molecular analysis of extragonadal YSTs is recommended to provide further insights into prognosis and treatment strategies.
Keywords: Yolk sac tumour, SMARCB1/INI1 deficiency, Head and neck neoplasms, Pediatric germ cell tumour Extragonadal tumour
RADIATION-INDUCED ADENOCARCINOMA OF THE SEMINAL VESICLE: DISTINCT ETIOLOGY AND UNIQUE IMMUNOHISTOCHEMICAL PROFILE
Yayuan Zhao MD PhD (University of Saskatchewan, Saskatoon, Canada; University of British Columbia, Vancouver, BC, Canada), Ren Yuan MD PhD (Department of Radiology, BC Cancer, Vancouver, BC, Canada; University of British Columbia, Vancouver, BC, Canada), Mehdi Agoumi MD (University of British Columbia, Vancouver, BC, Canada; Surrey Memorial Hospital, Surrey, BC, Canada), Chen Zhou MD PhD (University of British Columbia, Vancouver, BC, Canada; Department of Pathology, BC Cancer, Vancouver, BC, Canada), Gang Wang MD PhD (University of British Columbia, Vancouver, BC, Canada; Department of Pathology, BC Cancer, Vancouver, BC, Canada)
Objective: This study aims to assess the diagnostic challenges of primary adenocarcinoma of the seminal vesicles (PSVA), a rare and aggressive tumour, while highlighting the distinguishing factors that help differentiate it from secondary carcinomas. Additionally, it proposes an alternative pathway, characterized by distinct immunoprofiles.
Method(s): A thorough review of the literature was conducted. Microscopic examination of cytological features and radiological imaging for lesion localization were employed in the diagnostic process. Additionally, Immunohistochemical markers, including cytokeratin subsets 7 (CK7), cytokeratin subsets 20 (CK20), paired box 8 (PAX8), and others, were assessed as potential diagnostic tools.
Data and Results: PSVA is extremely rare, with fewer than 100 cases documented worldwide. It is associated with a high mortality rate and a poor prognosis. Accurate differentiation of PSVA is essential for proper diagnosis and treatment. Immunohistochemical markers, such as CK7 positivity, CK20 negativity, and PAX8 positivity, have proven useful. However, in our case, a 76-year-old male patient who had undergone long-term brachytherapy for prostatic adenocarcinoma developed seminal vesicle adenocarcinoma. Radiological studies confirmed the primary nature of the lesion. Immunohistochemical analysis revealed an interesting pattern: positive CK20, patchy CK7 positivity, and negative PAX8.
Conclusions: Immunohistochemical markers are valuable tools for the diagnosis of PSVA. Our case presents a distinct subtype of primary mucinous adenocarcinoma originating from the seminal vesicle, marked by a unique clinical history and immunohistochemical profile. This case may suggest an alternative progression pathway and etiology for PSVA, expanding the spectrum of this rare carcinoma.
Keywords: Keywords: Mucinous Adenocarcinoma, Seminle Vesicle, Radiation Induced
REASSESSING PD-L1 TESTING IN CERVICAL HPV-ASSOCIATED SQUAMOUS CELL CARCINOMA: A CASE FOR STREAMLINING PEMBROLIZUMAB ELIGIBILITY
Miryam Al Nasir (Department of Pathology, McGill University Health Centre, Montreal, Quebec, Canada), Gaelle Akiki (Department of Pathology, McGill University, Montreal, Quebec, Canada), Ajay Rajaram (Department of Pathology, McGill University Health Centre, Montreal, Quebec, Canada), Sarah Diwan (Department of Pathology, McGill University, Montreal, Quebec, Canada), Samirah Ghandurah (Department of Pathology, McGill University Health Centre, Montreal, Quebec, Canada), Mohamed Zakaria Bachir Bouyadjera (Faculté de pharmacie, Université de Montréal, Quebec, Canada), Anjelica Hodgson (Laboratory Medicine Program, University Health Network, Toronto, Ontario, Canada; Department of Laboratory Medicine and Pathobiology, Temerty Faculty of Medicine, University of Toronto, Ontario, Toronto, Canada), Basile Tessier-Cloutier (Department of Pathology, McGill University Health Centre, Montreal, Quebec, Canada; Department of Pathology, McGill University, Montreal, Quebec, Canada)
Objective: Treatment of recurrent/metastatic cervical cancer with pembrolizumab requires assessment of PD-L1 expression; however, this testing incurs additional costs, is subject to misinterpretation, and may, in some cases, delay treatment initiation. The threshold for PD-L1 positivity in cervical cancer is low and this study evaluates the level of expression across the spectrum of cervical neoplasia.
Methods: In a series of cervical malignancies, PD-L1 immunohistochemical (IHC) expression was assessed using the PD-L1 IHC 22C3 pharmDx assay. Positivity was defined as a combined positive score (CPS) ≥1. The subgroups included: HPV-associated squamous cell carcinoma (HPVa-SCC), HPV-independent squamous cell carcinoma (HPVi-SCC), HPV-associated non-SCC (HPVa-nonSCC), and HPV-independent non-SCC (HPVi-nonSCC). PD-L1 expression rates were compared across subgroups using chi-squared test and Student’s t-test.
Data and Results: All HPVa-SCC carcinomas (n=47) and HPVi-SCC (n=1) were PD-L1 positive while three PD-L1 negative cases were identified among the HPVa-nonSCC (1/15) and HPVi-nonSCC (2/6). The rate of PD-L1 positivity was significantly higher in HPVa-SCC when compared to the other subgroups combined (p< 0.01). The average PD-L1 CPS in HPVa-SCC (CPS 39) was higher than the other subgroups combined (CPS 24), though this difference was not statistically significant (p>0.05).
Conclusion: These findings support a reassessment of PD-L1 testing requirements for pembrolizumab eligibility in cervical cancer. While the limited number HPVa-nonSCC limit the interpretation in this subgroup, the absence of PD-L1 negative HPVa-SCC — representing the vast majority of cervical cancers — suggests that routine PD-L1 testing in this subset may be unnecessary. For now, PD-L1 testing remains informative for HPV-independent malignancies, particularly in the context of limited case numbers.
Keywords: Cervical cancer, immunohistochemistry, PD-L1, pembrolizumab
REVITALIZING AUTOPSY EDUCATION: A RETROSPECTIVE REVIEW OF A LARGE CANADIAN ACADEMIC CENTRE TO GUIDE EDUCATIONAL IMPROVEMENTS
J Nicole House (Department of Pathology and Laboratory Medicine, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada; Alberta Precision Laboratories, Calgary, AB, Canada), Amy Bromley (Department of Pathology and Laboratory Medicine, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada; Alberta Precision Laboratories, Calgary, AB, Canada)
Objective: Medical autopsy is a unique learning experience due to the breadth of entities and required clinical knowledge to make informed opinions. The introduction of Competency Based Medical Education raised questions regarding the number and breadth of exposures residents need. There is little published data regarding which disease entities residents routinely encounter. Our aim was to gather comprehensive data to identify potential gaps in the resident autopsy experience to enable evidence-informed improvement of residency education.
Methods: A retrospective review of the Calgary Autopsy Service was conducted spanning 4 academic years (July 1, 2017 to June 30, 2021). All hospital-based cases involving a pathology resident on their core autopsy rotations were included. Pediatric, central nervous system only, and on-call autopsies were excluded. Ethics approval: University of Calgary Conjoint Health Ethics Board (REB21-1408).
Results: Of the 772 autopsies performed, 432 included a resident, with each resident completing an average of 16.6 (± 4.4) cases. The most frequent natural causes of death for residents included atherosclerotic cardiovascular disease (ASCVD), sepsis/infection, malignancy, primary pulmonary disease, post-operative complications, and renal failure. There was major variability between residents regarding their exposure to these entities except ASCVD.
Conclusion: This study identified areas residents were not exposed to during their autopsy rotations, and highlights the need for a complementary robust, non-service based spiral curriculum to ensure foundational knowledge in all pertinent pathologies. In addition to disease processes inclusion of critical topics such as patient safety and health equity is mandatory to ensure competence in adult medical autopsy.
Keywords: Autopsy, residency education
SCLEROSING MUCOEPIDERMOID CARCINOMA WITH EOSINOPHILIA OF THE PAROTID GLAND: A CASE REPORT AND REVIEW OF THE LITERATURE
Adam Chen (Department of Biology at Gannon University, Erie, PA), Emma Zhang (Williamsville North High School, Amherst, NY), Keith Krabill, MD (Department of Pathology and Anatomical Sciences, University at Buffalo, Buffalo, NY), Frank Chen, MD, PhD (Department of Pathology and Anatomical Sciences, University at Buffalo, Buffalo, NY)
Sclerosing mucoepidermoid carcinoma with eosinophilia (SMECE) is an exceptionally rare malignant tumour in the salivary gland, as a diagnostically challenging entity in the salivary gland. While it shows mucoepidermoid differentiation, the lack of MAML2 translocation differentiates it from conventional mucoepidermoid carcinoma (MEC), suggesting it may be a distinct entity. To date, only 28 cases of SMECE have been reported in the salivary gland. The clinicopathological and molecular features of the tumour still remain unclear. Here, we report a case of a 41-year-old man with SMECE in his parotid gland. The patient presented a slowly growing right neck mass. Image study revealed a 3.7 cm complex cystic mass in the right parotid. The surgery was pursued after a non-diagnostic fine needle aspiration. Grossly, the tumour was a 3 cm tan nodule with minimal attached soft tissue. Microscopically, the tumour is relatively well demarcated with anastomosing lobules of neoplastic cells with fibrotic stroma rich in lymphoplasmacytosis and eosinophils. Focal glandular differentiation was confirmed by mucicarmine stain. Immunohistochemically, the tumour cells are diffuse positive for pancytokeratin and p40. The tumour is negative for MAML2, EWSR1, and FUS rearrangements, reinforcing its distinct pathogenesis from conventional MEC and other salivary gland neoplasms. SMECE can be confused with chronic sclerosing sialadenitis, lymphoepithelial carcinoma, or other inflammatory/reactive conditions due to its dense fibroinflammatory background. This case contributes to the limited literature on SMECE, emphasizing its diagnostic difficulty and potential for misclassification. Further clinicopathological and molecular studies are needed to better understand its pathogenesis, prognosis, and therapeutic implications.
Keywords: Sclerosing mucoepidermoid carcinoma with eosinophilia (SMECE)
SIMULATION-BASED MEDICAL EDUCATION IN POSTGRADUATE PATHOLOGY TRAINING: A SCOPING REVIEW
Laura Lockau (Department of Pathology and Laboratory Medicine, Schulich School of Medicine and Dentistry, Western University, Canada), Emily Goebel (Department of Pathology and Laboratory Medicine, Schulich School of Medicine and Dentistry, Western University, Canada), Christopher Tran (Department of Pathology and Laboratory Medicine, Schulich School of Medicine and Dentistry, Western University, Canada)
Background: Simulation-based medical education (SBME) is a form of experiential learning that uses simulation aids in place of real patients to replicate clinical scenarios. Literature on SBME in postgraduate training has largely focused on clinical specialties, where these techniques have been used to build procedural skills. To date, no study has comprehensively reviewed SBME applications in postgraduate pathology training.
Methods: We searched 6 databases (Medline, Embase, Cochrane library, Web of Science, ERIC, and Scopus) from inception to July 2023. Inclusion and exclusion criteria were applied during title/abstract screening and subsequent full text review by two independent reviewers.
Results: We included 25 studies focusing on SBME in pathology postgraduate training. Most studies were published as conference abstracts (n=15), with fewer primary research articles (n=8) and review articles/chapters (n=2). Common areas of focus included microscopic examination (n=10), clinician-pathologist communication (n=5), frozen section (n=4), grossing (n=4), quality assurance (n=2), molecular pathology (n=1), and on-call responsibilities (n=1). No study explicitly defined the term “simulation,” and interventions varied widely from the use of online modules with whole-slide images, to communication role-play scenarios, to physical specimen models. Only one study examined a Canadian context.
Conclusions: SBME has been used to enhance teaching in multiple areas of postgraduate pathology training. Available literature on the use of simulation in pathology education is, however, limited by the small number of studies, the variable application and lack of standardized definition of “simulation,” and the predominance of conference abstracts containing limited detail on the interventions used and outcome data produced.
Keywords: Medical education; Simulation; Postgraduate pathology training; Scoping review
SPINAL AXIS MAPPING OF IMMUNOHISTOCHEMICAL (IHC) ALPHA-SYNUCLEIN IN PARKINSON’S DISEASE AUTOPSY SERIES
Pramath Kakodkar (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Javera Tariq (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Ali H. Rajput (Movement Disorders Program, Division of Neurology, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Alex Rajput (Movement Disorders Program, Division of Neurology, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Roland N. Auer (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada)
Objective: Braak and colleagues (2003) proposed an influential albeit debated model outlining alpha-synuclein (α-Sn) migration in a predictable caudo-rostral pattern, from peripheral/autonomic compartment to spinal cord. We mapped the spinal cord with α-Sn immunohistochemistry (IHC) on a Parkinson’s disease (PD) autopsy series to determine if the Lewy inclusion burden is highest in the sacral (supporting caudo-rostral spread) or cervical (suggesting alternate routes) sections.
Methodology: From 2016-2021, all autopsies with well-established PD (n=35) were included. The cervical, thoracic, lumbar and sacral levels were sectioned and stained with Anti-phospho-Ser129 α-Sn antibodies to identify Lewy inclusions (Lewy bodies (LB), Lewy neurites (LN), and granular α-Sn (GA)). These were mapped according to functional Rexed groups and semi-quantitative scored (0: No Lewy inclusion, 1: sparse Lewy inclusion (1-2/10×), 2: moderate Lewy inclusion (3-10/10×), 3: Dense Lewy inclusion (>10/10×).
Results: Lewy inclusions scores showed similar distribution across all spinal levels (mean: 0.8, Friedman χ²≈3.33, p=0.19). Case-level progression analysis showed minimal caudo-rostral and rostro-caudal progression across consequent spinal levels. No change pattern was most common across all morphologies (LB:40%, LN:71%, GA:63%). Functional Rexed lamina analysis demonstrated that autonomic regions had significantly higher Lewy inclusion scores across all levels (p< 0.01).
Conclusion: Our study suggests heterogeneity in spinal α-synuclein pathology as there was no Lewy inclusion distribution gradient seen. Predilection for autonomic regions for all Lewy inclusions explains early autonomic symptoms in PD as such autonomic circuits must be considered as a target for future biomarker development or therapy. Overall, our findings lend no support to Braak’s caudo-rostral hypothesis of PD.
Keywords: Parkinson’s Disease, Alpha-synuclein, Spinal cord, Lewy Body, Caudo-rostral
THE DIAGNOSTIC AND CLINICAL PATHOLOGY RESIDENT ON-CALL: IMPROVING RESIDENT EDUCATIONAL EXPERIENCES WITH A RETROSPECTIVE REVIEW OF ON-CALL FREQUENCY AND TRENDS
Daniel J Markewich (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada), Pramath Kakodkar (Department of Pathology and Laboratory Medicine, University of Saskatchewan and Saskatchewan Health Authority, Saskatoon, SK, Canada)
Objective: The Diagnostic and Clinical Pathology (DCP) residents at the University of Saskatchewan cover call over one-week intervals beginning at 17:00 hours on Friday and ending at 08:00 hours the following Friday. This includes weekend coverage from Friday evening until Monday morning and weekday coverage from 17:00 until 08:00 hours. DCP resident on-call provides simultaneous coverage for Anatomical Pathology, Microbiology, Biochemistry, Hematopathology, and Transfusion Medicine. Residents had anecdotally noticed an overall increase in the daily number of pages. Therefore, residents took the initiative to audit our on-call trends.
Methods: This was a retrospective review of call data over 2024. Data collected included the resident, date and time of page, relevant service, amount of time resolving the page, and amount of time in the hospital. Data were then analyzed with descriptive statistics.
Results: Residents were actively working an average of 13.6 ± 4.3 hours over a cumulative weekend and 8.5 ± 3.8 hours over a cumulative weekday shift. Additionally, residents spent an average of 10.4 ± 4.2 hours in the hospital during their call shifts. The majority of pages came from the Microbiology service with residents receiving 29 ± 8 pages representing 56% of their total calls. Anatomical Pathology, Hematopathology, and Microbiology were the three most time-consuming services, with weekly calls accounting for 2.9 ± 2.5 hours, 6.9 ± 2.6 hours, and 7.8 ± 4.4 hours, respectively.
Conclusions: The DCP call coverage exceeded the recommended “Home Light” call designation as per the Resident Doctors of Saskatchewan (RDoS) and Post-Graduate Medical Education (PGME). Therefore, efforts were made to re-designate DCP call as “Home Heavy” and re-organize our call schedule in to more palatable shorter, but more frequent call shifts.
Keywords: Resident Education, On-Call, Diagnostic and Clinical Pathology
THE ISOLATED ‘TRUE’ RETROPERITONEAL CYST €" A CLINICOPATHOLOGICAL AND IMMUNOHISTOCHEMICAL STUDY OF THREE CASES WITH IMPLICATIONS FOR MULTIFACETED HISTOGENESIS
Bryan Johnston (Department of Pathology and Laboratory Medicine, College of Medicine, University of Saskatchewan, Saskatoon, SK), Pramath Kakodkar (Department of Pathology and Laboratory Medicine, College of Medicine, University of Saskatchewan, Saskatoon, SK), Nick Baniak (Department of Pathology and Laboratory Medicine, College of Medicine, University of Saskatchewan, Saskatoon, SK; Saskatoon City Hospital, Saskatchewan Health Authority, Saskatoon, SK), Rani Kanthan (Department of Pathology and Laboratory Medicine, College of Medicine, University of Saskatchewan, Saskatoon, SK; Royal University Hospital, Saskatchewan Health Authority, Saskatoon, SK)
Objective: Isolated ‘true’ epithelial-lined retroperitoneal cysts unrelated to solid organs are rare and usually asymptomatic. We present three cases encountered on imaging for abdominal/back pain.
Methods:
Case 1: 66-year-old male imaged for abdominal/back pain identified a 4.7 x 3.4 cm retroperitoneal cyst. Pathology confirmed variable-sized cysts with a histological triad of lymphoepithelial cysts [D240/CD31+ve ], smooth muscle in fibrous stroma [SMA/Desmin+ve], and lymphoid aggregates.
Case 2: 35-year-old female imaged for an obstructing splenic mass identified a 3.8 x 2.3 cm cystic lesion in the left paracolic gutter. Pathology identified a thin-walled unilocular cyst lined by predominantly cuboidal-to-columnar epithelium with abundant ‘mucin-like’ cytoplasm [LMKT, CK7, PAX8, ER/PR+ve; negative Calretinin/WT1] interspersed with a flattened single mesothelial cell-lined layer [Calretinin/WT1+ve; negative PAX8/ER/PR]. No expression of CDX2/CK20/D240 and mucicarmine/PAS/PASD showed a gradient staining pattern.
Case 3: 53-year-old male with a retroperitoneal cystic lesion identified on surveillance imaging for testicular cancer. Pathology identified a 10 cm multiloculated smooth cyst containing gelatinous mucoid material. The cyst was lined by mucinous epithelium in papillations with goblet cells [CK20/CDX2+ve; mucicarmine/PASD rich staining; negative Calretinin/D240/WT1/ PAX8/ER/PR].
Results:
Case 1: Retroperitoneal Multicystic Lymphangioma
Case 2: Retroperitoneal cyst with Mesothelial and Müllerian differentiation with mucinous metaplasia
Case 3: Retroperitoneal Enterogenous cyst
Conclusions: Retroperitoneal cystic lesions present a diagnostic dilemma due to their silent nature and critical anatomy. A multidisciplinary team approach is essential for accurate diagnosis and management. Despite their ‘embryological/congenital’ origin, they remain poorly understood in adults. Their rarity, diverse etiologies, and ambiguous classification underscore the need for ongoing investigation.
Keywords: Epithelial cyst, Retroperitoneal cyst, Mesothelial cyst, Müllerian differentiation, Immunohistochemistry
THE RAREST EPITHELIAL-MYOEPITHELIAL LESION OF THE BREAST: A CASE OF MALIGNANT ADENOMYOEPITHELIOMA (AME-M)
Rebecca J. Brassington [Department of Laboratory Medicine and Pathology, University of Alberta, Edmonton, AB, Canada], Svetlana Silverman [Department of Laboratory Medicine and Pathology, University of Alberta, Edmonton, AB, Canada; Misericordia Community Hospital, Edmonton, AB, Canada]
Background: Adenomyoepitheliomas (AME) of the breast are characterized by dual differentiation with luminal and myoepithelial cells. Malignant AME (AME-M) can arise from the epithelial, myoepithelial or both components and occur most frequently in elderly women. AME-M are exceptionally rare and no data on incidence have been reported; AME-M have only been described in case reports and small case series.
Case Presentation: An 86-year-old woman presented with a left breast mass growing over 3-4 years and peau d’orange and was found to have an irregular mass (5 cm) with microcalcifications. Core biopsies demonstrated triple-negative carcinoma. She was treated with mastectomy and axillary dissection, revealing AME-M with negative lymph nodes and clear margins. There is no evidence of disease at 5 months.
Discussion: Two patterns of AME-M have been described, with neoplasms consisting of typical AME merging with areas of malignant cells or tumours with the overall architecture of an AME but have foci of increased mitoses, necrosis and atypia. This is a case of a tumour of the former pattern, consisting of AME with metaplastic carcinoma with features of squamous cell carcinoma.
Conclusions: AME-M are exceptionally uncommon and further awareness and characterization of this entity can aid understanding and identification.
Keywords: Adenomyoepithelioma, Malignant Adenomyoepithelioma, Epithelial-Myoepithelial lesions, Metaplastic Carcinoma, Breast pathology
ARCHITECTURAL PATTERNS IN HEPATOCELLULAR CARCINOMA ARE ASSOCIATED WITH DISTINCT EPIGENETIC STATES
Isabella Xiao (University of Alberta), Rebecca Phillips (University of Alberta), Venancio Avancini Ferreira Alves (University of Sao Paulo), Sebastiao N Martins-Filho (University of Alberta)
Objective: To investigate whether architectural patterns in hepatocellular carcinoma (HCC) are associated with specific epigenetic features.
Design/Methods: We evaluated 307 HCC samples from the Cancer Genome Atlas (TCGA), classifying tumours as low-grade (LG; pseudoacinar and trabecular ≤4 cells thick, n = 137) or high-grade (HG; solid or trabecular >4 cells thick, n = 170) based on architectural patterns. Differential mutation and methylation analyses were performed, and genes were annotated using databases of oncogenes and tumour suppressor genes (TSGs).
Results: HG tumours were associated with worse overall and disease-free survival (p< 0.01). TP53 was the only gene with a significantly higher mutation frequency in HG versus LG tumours (adjusted p< 0.001). Methylation analysis revealed hypomethylation of numerous oncogenes in HG tumours. Surprisingly, several tumour suppressor genes (TSGs) were also hypomethylated, suggesting a possible global hypomethylation state. Notably, when only TP53 wild-type tumours were analyzed, IGF2 and SQSTM1, genes associated with cell proliferation and autophagy dysregulation in HCC, remained significantly hypomethylated. These findings suggest that while TP53 mutation may amplify epigenetic disruption, architectural patterns may still reflect distinct epigenetic programs independent of TP53 status.
Conclusion: Histological architectural patterns in HCC are associated with distinct DNA methylation profiles, clinical outcomes, and TP53 mutation status. Even in the absence of a TP53 mutation, architecture identifies tumours with important epigenetic alterations in the context of HCC, supporting the potential of routine morphological evaluation to provide insights into underlying tumour biology.
Keywords: Hepatocellular carcinoma, DNA methylation, morphomolecular correlates
UNUSUAL GENE FUSIONS IN PEDIATRIC NODULAR FASCIITIS: A CASE SERIES
Aida I Glembocki (The Hospital for Sick Children), Robert I Siddaway (The Hospital for Sick Children), Anthony Arnoldo (The Hospital for Sick Children), Gino R Somers (The Hospital for Sick Children )
Background: Nodular fasciitis (NoF) is a benign myofibroblastic proliferation that usually occurs in the subcutaneous tissues of the upper extremities, trunk, as well as head and neck in young adults, with fewer than 10% of cases presenting in childhood. The USP6 gene fusion detection, with the MYH9 gene as the most common fusion partner, has been proven as a useful diagnostic tool in cases with morphological uncertainty. The reported list of alternative fusion partners and their clinical correlations has expanded in recent years.
Objective: We aim to characterize six pediatric cases of NoF through histopathology, immunohistochemistry, and a targeted RNAseq assay, which revealed three examples of less common fusion partners with USP6.
Design: Archival material from pediatric patients (n=6) diagnosed with NoF from 2019 to 2023 was retrieved. The clinicopathological features and molecular findings were reviewed.
Results: The table summarizes the clinical and molecular features. All cases examined showed typical histomorphology and were diffusely positive for smooth muscle actin.
Conclusion: In 3 of 6 (50%) cases in this study, the most common MYH9::USP6 gene fusion was detected. The remaining 3 cases represented unusual USP6 fusion partners such as SPARC, COL1A1 and RRBP1. The SPARC::USP6 gene fusion has been reported previously in a NoF of the temporal region in a girl in middle childhood. In contrast, COL1A1::USP6 and RRBP1::USP6 gene fusions are more ubiquitous. COL1A1::USP6 is predominant in ossifying lesions like fasciitis ossificans and myositis ossificans and contributes to a small subset of NoF cases. The RRBP1::USP6 gene fusion has been reported both in NoF and low-grade myofibroblastic sarcoma in a thigh lesion in a 29-year-old female. In lesions with this fusion, the morphology becomes important, particularly if margins are positive, as it is the only criterion to differentiate NoF from a low-grade myofibroblastic sarcoma, which is prone to local recurrence.
Keywords: Nodular fasciitis, molecular pathology, pediatric pathology
UNVEILING THE UNCOMMON: A CASE REPORT OF PRIMARY ENDOMETRIAL SQUAMOUS CELL CARCINOMA
Javera Tariq, Joel Scott, Nicholas Baniak, Marilyn Kinloch
Introduction: Primary endometrial squamous cell carcinoma (PESCC) is an exceptionally rare subtype of endometrial cancer. Our case report presents a unique case of HPV-independent PESCC.
Clinical Presentation: A 75-year-old female presented with postmenopausal bleeding. Subsequent endometrial and cervical biopsies showed atrophic cervical mucosa with inflammation but were negative for intraepithelial dysplasia or malignancy. However, endometrial biopsies obtained simultaneously revealed HPV-independent invasive squamous cell carcinoma with negative P16 and mutant P53. Identifying the origin of the tumour on biopsy was significantly challenging. A total abdominal hysterectomy and bilateral salpingo-oophorectomy with lymph node dissection and omentectomy were then performed. Microscopic examination revealed complete replacement of the endometrial surface with squamous epithelium (ichthyosis uteri), P16, HPV-ISH negative, P53 mutant (null), and ER-negative, confirming the above diagnosis. The carcinoma was deeply invasive, originating from the surface and infiltrating 97% of the myometrium. The tumour also involved the lower uterine segment and upper endocervix. The remainder of the cervix was atrophic and uninvolved. Additionally, extensive lymphovascular invasion was noted. The fallopian tubes, ovaries, omentum, and lymph nodes were negative for malignancy. MMR was intact.
Results: This case of HPV-independent squamous cell carcinoma posed a significant diagnostic challenge regarding the origin of the tumour. In the absence of cervical mucosal involvement and given the extensive endometrial surface involvement, PESCC was favored. The entire uterus and cervix were meticulously evaluated, and an endometrioid carcinoma with extensive squamous differentiation was also considered a differential diagnosis.
Conclusion: PESCC, a rare and challenging entity, was first reported in the literature in 1982. To our knowledge, only approximately 100 cases have been documented to date, making it a difficult diagnosis. Currently, there are no standardized treatment guidelines tailored explicitly for this tumour. However, as more cases are documented, there is potential for the development of specific treatment protocols.
Keywords: Endometrial, squamous, carcinoma
WHEN LESS IS MORE: A RETROSPECTIVE ANALYSIS OF OUT-OF-CONTROL VITAMIN TESTING IN SASKATCHEWAN
Hasan Jamil BHSc (College of Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Department of Pathology & Lab Medicine, Saskatchewan Health Authority, Saskatoon, SK, Canada), Fang Wu PhD DABCC FCACB FAACC (College of Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Department of Pathology & Lab Medicine, Saskatchewan Health Authority, Saskatoon, SK, Canada), Pouneh Dokouhaki PhD MD FRCPC (College of Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Department of Pathology & Lab Medicine, Saskatchewan Health Authority, Saskatoon, SK, Canada), Ahmed Mostafa PhD MD D(ABHI) F(ACHI) (College of Medicine, University of Saskatchewan, Saskatoon, SK, Canada; Department of Pathology & Lab Medicine, Saskatchewan Health Authority, Saskatoon, SK, Canada)
Objective: Testing for vitamins D and B12 is commonly ordered by physicians globally despite their limited testing indications. This project described and analyzed testing patterns in the former Saskatoon Health Region.
Design/Methods: Deidentified data from the Saskatoon Hospital Laboratory Information System from Jan. 1st, 2018, to Dec. 31st, 2022, was analyzed and visualized with Microsoft Excel. Collected metrics included total number of tests ordered along with breakdown by city, physician type, and test result, as well as analysis of repeat tests.
Results: From 2018 to 2022, 110078 vitamin D and 192776 vitamin B12 tests were ordered in the former Saskatoon Health Region. Testing was greatest in rural areas, with the highest rate of vitamin B12 testing occurring in Nokomis (population 414, 3395 tests over 5 years) and the highest rate of vitamin D testing occurring in Davidson (population 1044, 900 tests over 5 years). The ten most frequently ordering physicians for each test were all family physicians except for one. 98% of all tests ordered had normal results. Repeat testing analysis within a calendar year showed 8177 people being tested at least twice for vitamin D and 19745 people for vitamin B12.
Conclusion: There is severe and worsening inappropriate testing in the region for vitamins D and B12. Statistical analysis revealed increasing volumes, inappropriate repeat testing, high proportions of normal results, and a small number of family physicians accounting for a high percentage of ordering. Potential future interventions may include laboratory requisition form changes, physician education materials, and physician-specific laboratory audit reports.
Keywords: Vitamin D, vitamin B12, choosing wisely, inappropriate testing, laboratory utilization

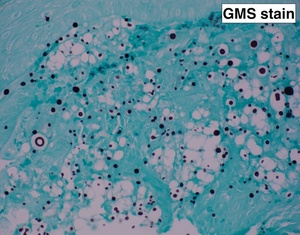
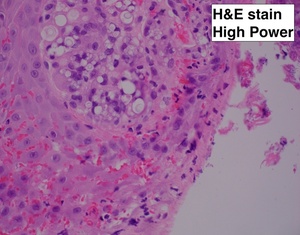
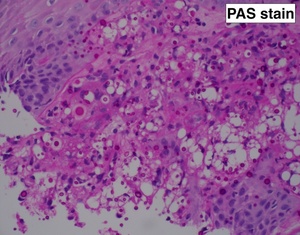
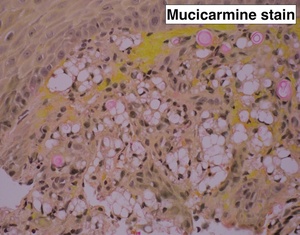

_the_lower_power_image_.png)
_a_lower_power_view_of_this_component_showing_solid.png)
_positive_staining_for_ini1._(b)_positive_staining_for_sf-1._(c)_positive_staining_for_.png)
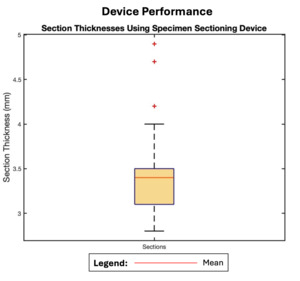
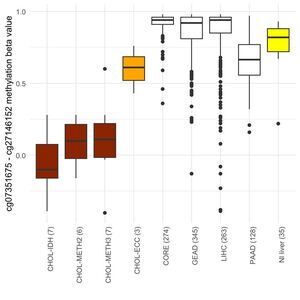
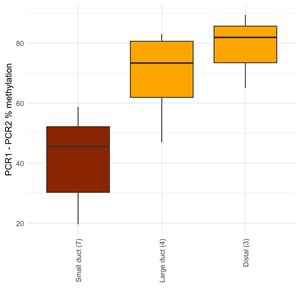
_results_for_patient__8__diagnosed_as_an_-thalassemia_(at)_si.png)
_results_for_patient__6__diagnosed_with_-thalassemia_(at)_tra.png)
_results_for_patient__4__consistent_with_-thalassemia_(at)_tr.png)
__afp_(no.png)



_seen_w.jpg)

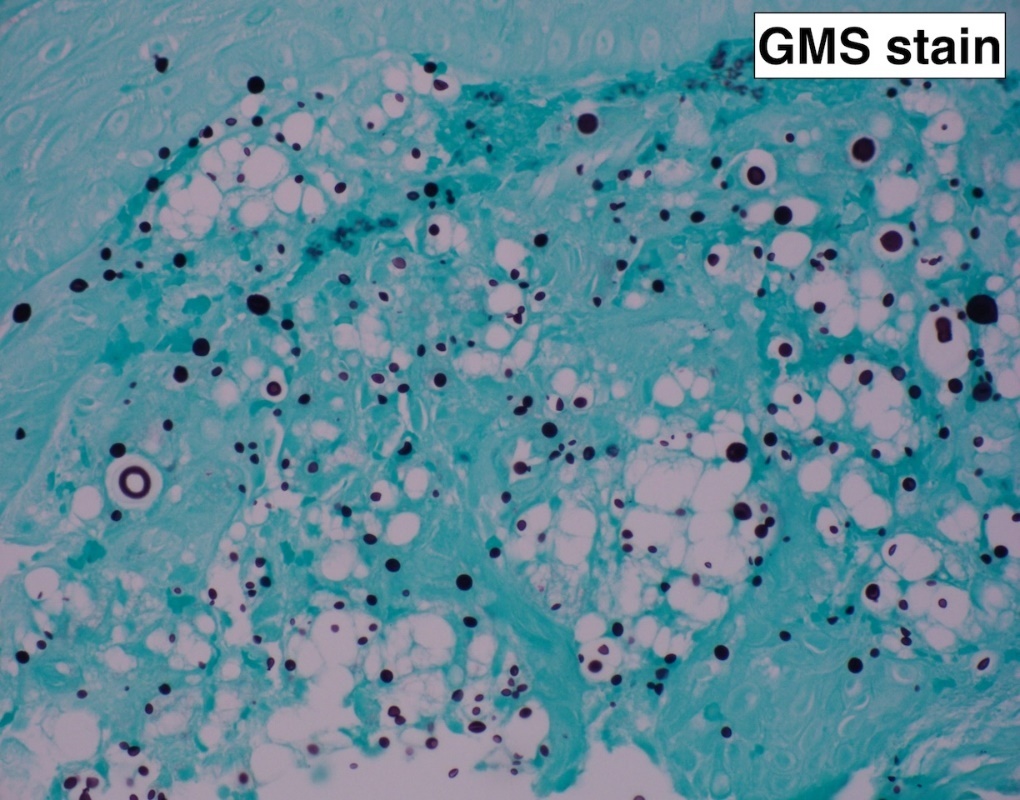
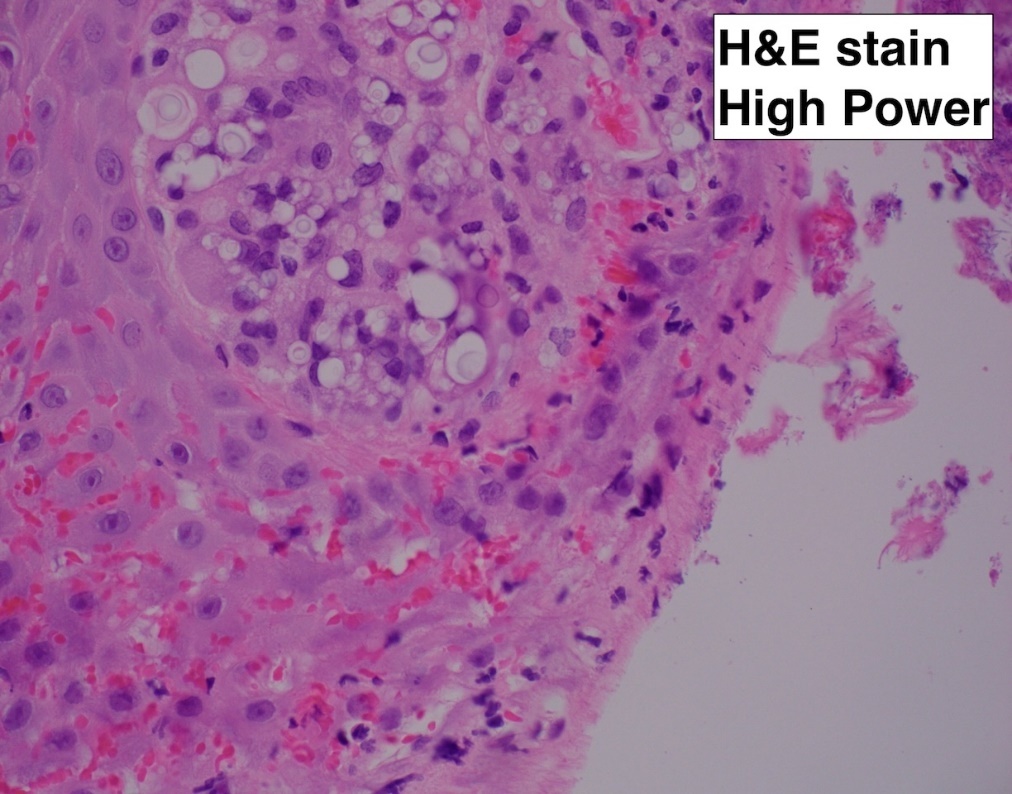
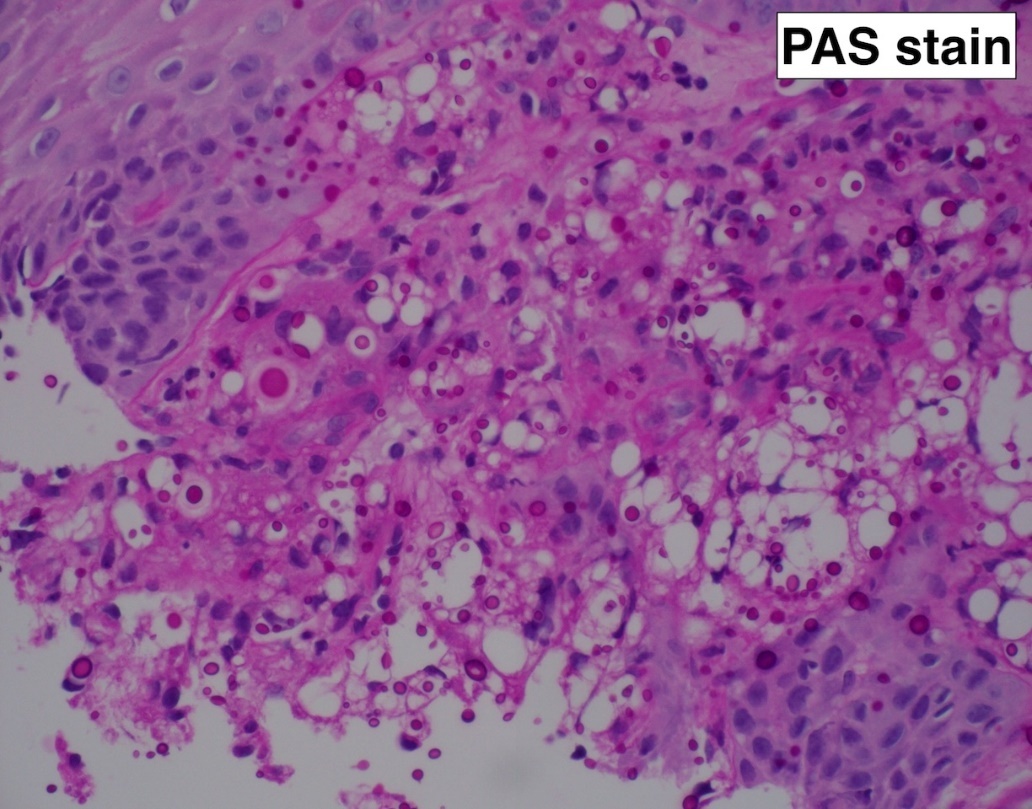
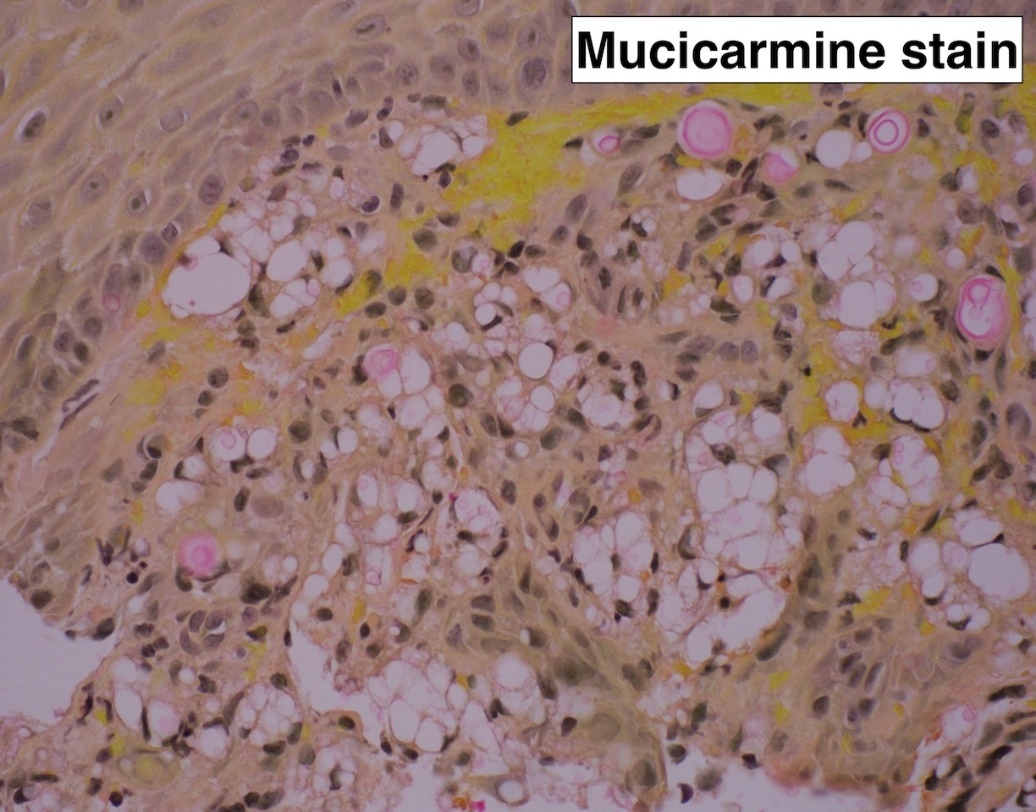

_the_lower_power_image_.png)
_a_lower_power_view_of_this_component_showing_solid.png)
_positive_staining_for_ini1._(b)_positive_staining_for_sf-1._(c)_positive_staining_for_.png)
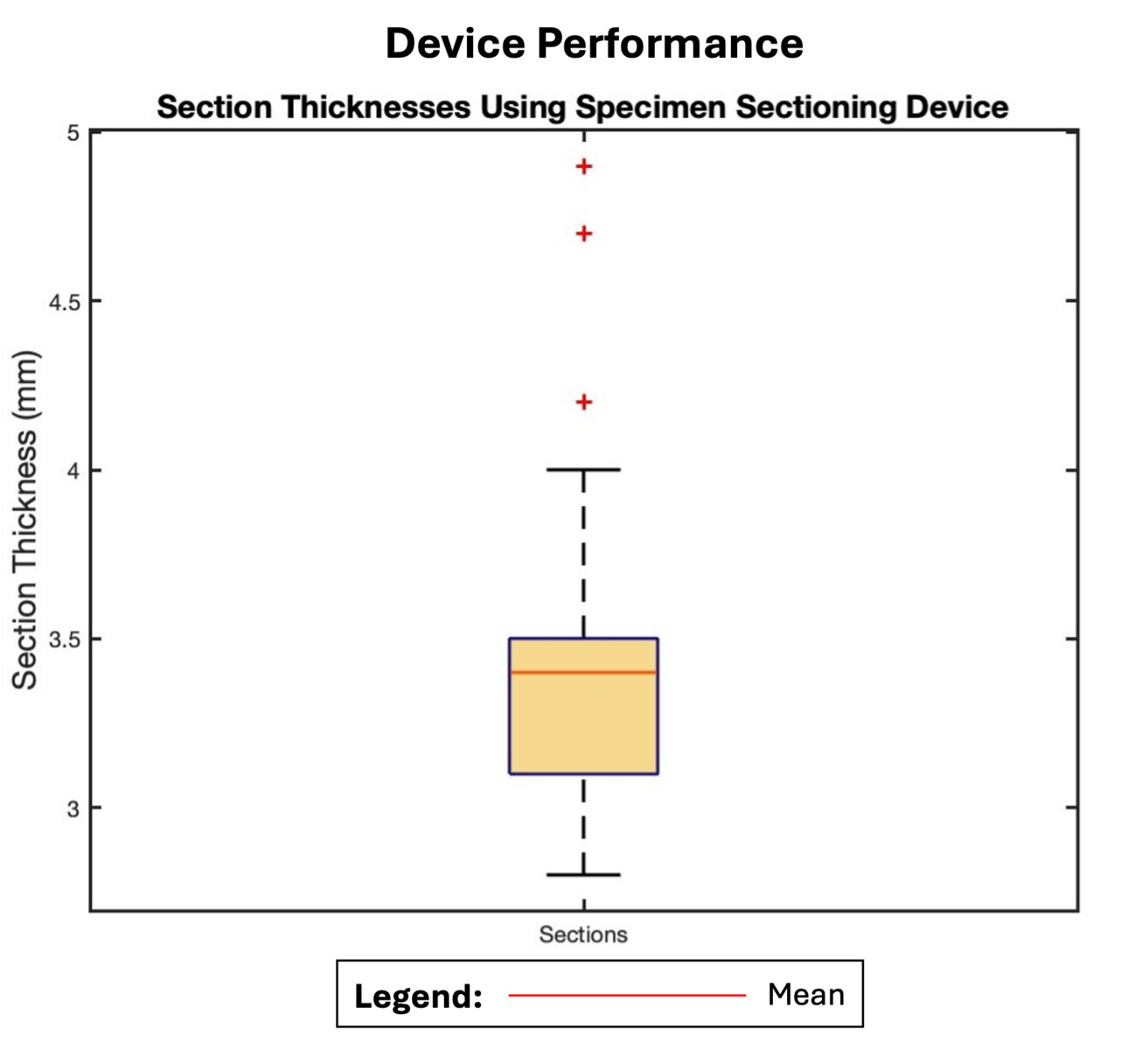
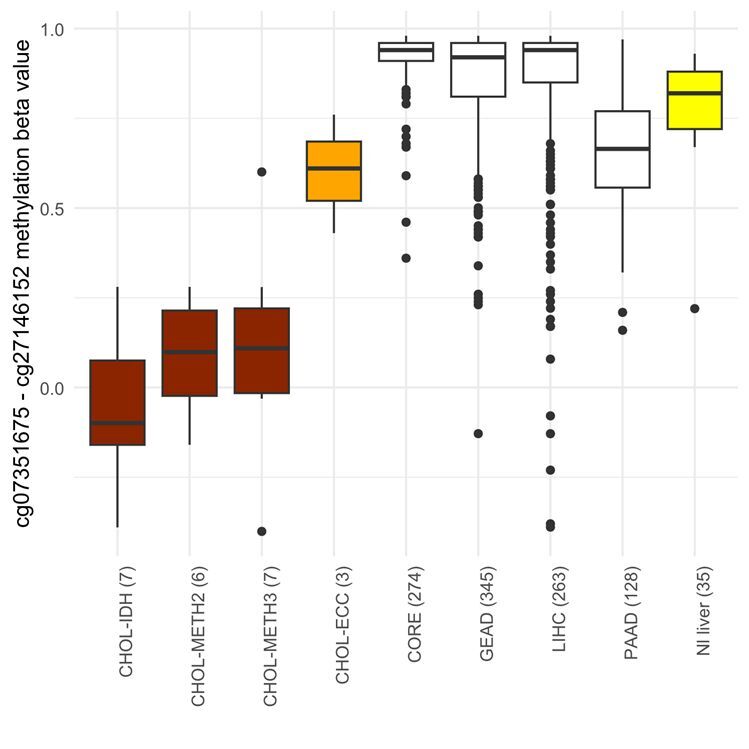
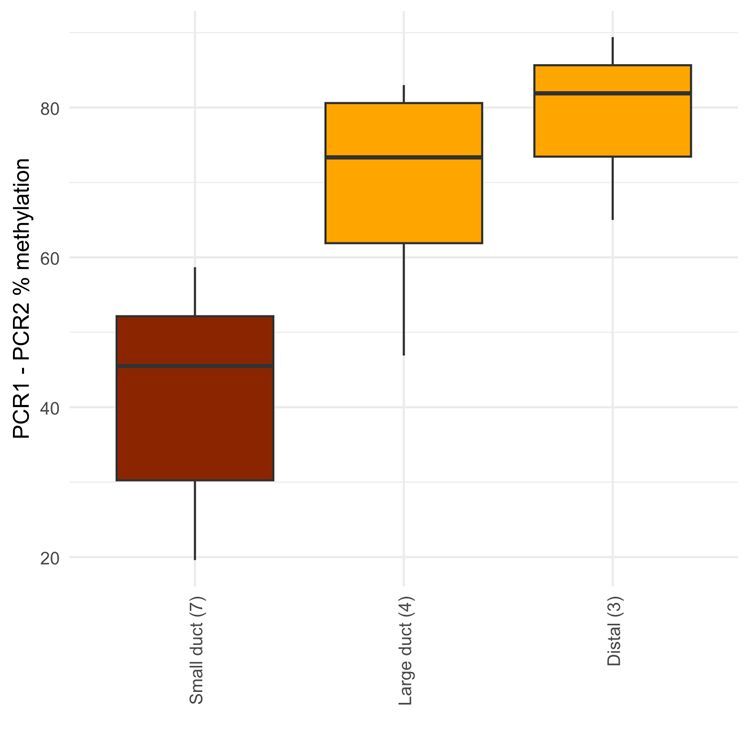
_results_for_patient__8__diagnosed_as_an_-thalassemia_(at)_si.png)
_results_for_patient__6__diagnosed_with_-thalassemia_(at)_tra.png)
_results_for_patient__4__consistent_with_-thalassemia_(at)_tr.png)
__afp_(no.png)
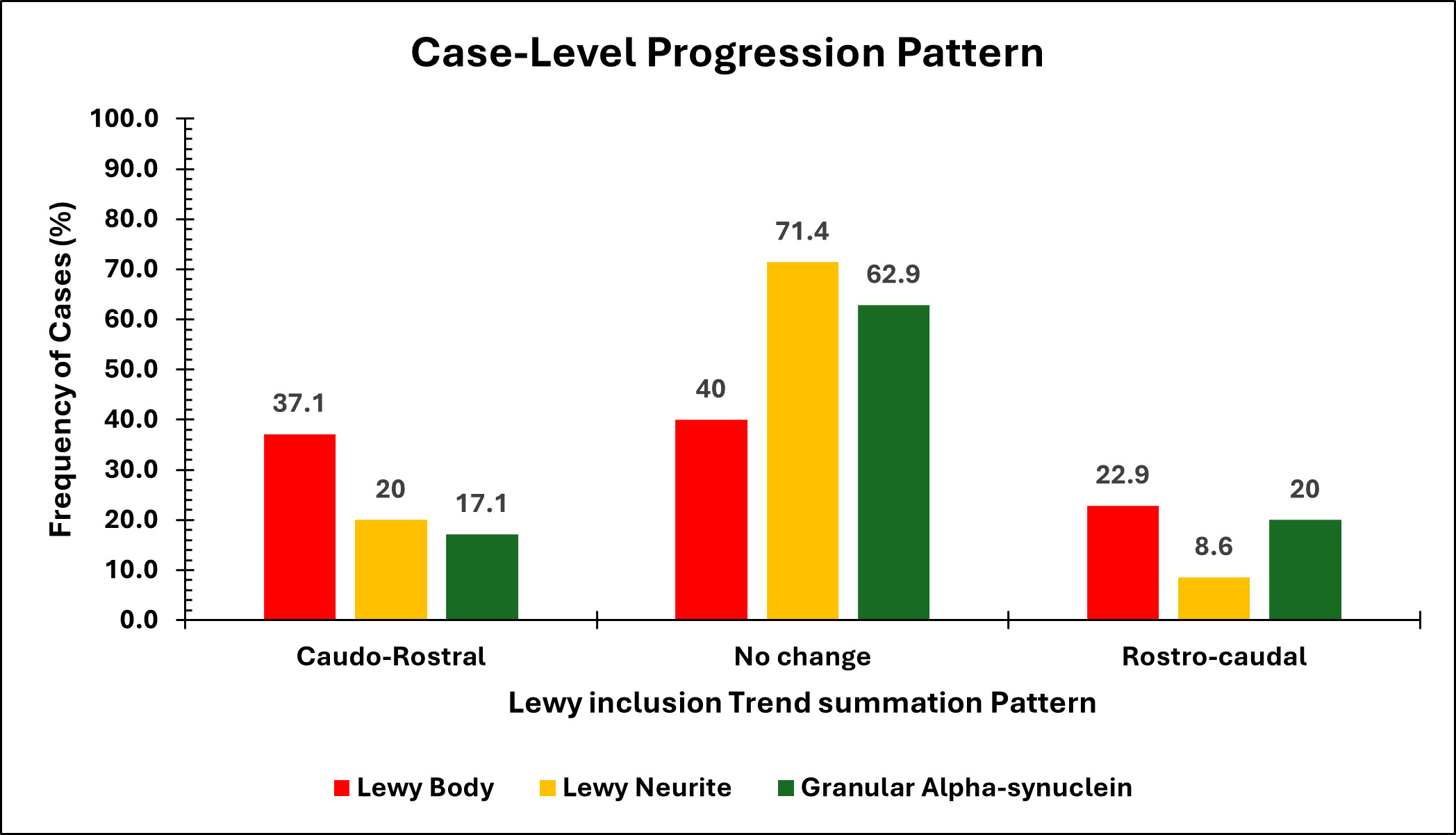
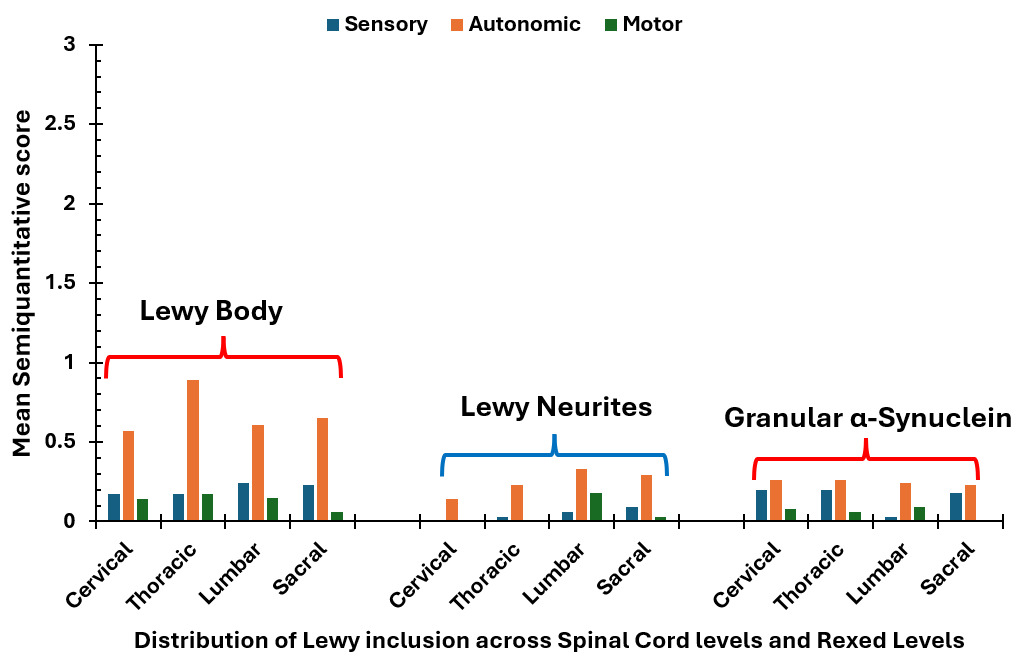

_seen_w.jpg)